Podcast
Questions and Answers
Which of the following is the most common type of skin cancer?
Which of the following is the most common type of skin cancer?
- Merkel Cell Carcinoma
- Basal Cell Carcinoma (correct)
- Melanoma
- Squamous Cell Carcinoma
Which of the following factors is least likely to be associated with an increased risk of Basal Cell Carcinoma?
Which of the following factors is least likely to be associated with an increased risk of Basal Cell Carcinoma?
- Chronic sun exposure
- Exposure to arsenic
- Genetic disorders
- Vitamin D deficiency (correct)
What percentage of Nevus Sebaceous lesions, present at birth on the scalp or face, are estimated to become Basal Cell Carcinoma?
What percentage of Nevus Sebaceous lesions, present at birth on the scalp or face, are estimated to become Basal Cell Carcinoma?
- 10% (correct)
- 50%
- 25%
- 5%
A patient presents with a skin lesion described as flush with the skin, erythematous, and scaly. It occasionally exhibits a shallow ulcer or crusting and is sometimes mistaken for eczema. Which type of Basal Cell Carcinoma is most likely?
A patient presents with a skin lesion described as flush with the skin, erythematous, and scaly. It occasionally exhibits a shallow ulcer or crusting and is sometimes mistaken for eczema. Which type of Basal Cell Carcinoma is most likely?
A flesh-colored nodule on the surface of the skin with small telangiectatic vessels coursing throughout, central depression and a peripheral rolled border is consistent with which clinical presentation?
A flesh-colored nodule on the surface of the skin with small telangiectatic vessels coursing throughout, central depression and a peripheral rolled border is consistent with which clinical presentation?
Which type of Basal Cell Carcinoma typically presents as a firm white or yellowish plaque with an ill-defined border, often described by patients as an enlarging scar?
Which type of Basal Cell Carcinoma typically presents as a firm white or yellowish plaque with an ill-defined border, often described by patients as an enlarging scar?
For a Basal Cell Carcinoma lesion with a low likelihood of recurrence in a high-risk area such as the central face, what is the maximum diameter generally considered acceptable for surgical removal?
For a Basal Cell Carcinoma lesion with a low likelihood of recurrence in a high-risk area such as the central face, what is the maximum diameter generally considered acceptable for surgical removal?
What is the approximate percentage of patients who have had one Basal Cell Carcinoma that will develop another lesion within 5 years?
What is the approximate percentage of patients who have had one Basal Cell Carcinoma that will develop another lesion within 5 years?
Surgical excision of Basal Cell Carcinoma with 4 to 5 mm margins has demonstrated what approximate 5-year cure rate?
Surgical excision of Basal Cell Carcinoma with 4 to 5 mm margins has demonstrated what approximate 5-year cure rate?
Which of the following treatment modalities is MOST appropriate for low-risk superficial Basal Cell Carcinomas on the trunk or extremities?
Which of the following treatment modalities is MOST appropriate for low-risk superficial Basal Cell Carcinomas on the trunk or extremities?
The PTCH1 gene, implicated in Basal Cell Carcinoma pathogenesis, functions primarily as a what?
The PTCH1 gene, implicated in Basal Cell Carcinoma pathogenesis, functions primarily as a what?
What is the role of the SMO protein in the context of the Hedgehog signaling pathway and Basal Cell Carcinoma development?
What is the role of the SMO protein in the context of the Hedgehog signaling pathway and Basal Cell Carcinoma development?
Compared to cutaneous Squamous Cell Carcinomas, P53 mutations are typically?
Compared to cutaneous Squamous Cell Carcinomas, P53 mutations are typically?
Radiation injury, chronic sun exposure, and chronic chemical exposure are primary etiologic factors for:
Radiation injury, chronic sun exposure, and chronic chemical exposure are primary etiologic factors for:
A patient presents with a rapidly growing lesion with a tendency for spontaneous resolution. Histological and clinical appearance are very similar to nodular squamous cell carcinoma. This is likely:
A patient presents with a rapidly growing lesion with a tendency for spontaneous resolution. Histological and clinical appearance are very similar to nodular squamous cell carcinoma. This is likely:
A chronic, unstable burn scar or chronic draining osteomyelitis can undergo premalignant changes leading to:
A chronic, unstable burn scar or chronic draining osteomyelitis can undergo premalignant changes leading to:
What characteristics describe Bowen's Disease?
What characteristics describe Bowen's Disease?
Untreated Squamous Cell Carcinomas, compared to Basal Cell Carcinomas, typically:
Untreated Squamous Cell Carcinomas, compared to Basal Cell Carcinomas, typically:
What is the approximate metastatic rate for actinically induced Squamous Cell Carcinomas?
What is the approximate metastatic rate for actinically induced Squamous Cell Carcinomas?
Following initial treatment for Squamous Cell Carcinoma, what is the recurrence rate if re-treatment is administered to achieve ultimate cure?
Following initial treatment for Squamous Cell Carcinoma, what is the recurrence rate if re-treatment is administered to achieve ultimate cure?
When is excision with frozen section pathologic diagnosis the preferred treatment for Squamous Cell Carcinoma?
When is excision with frozen section pathologic diagnosis the preferred treatment for Squamous Cell Carcinoma?
What is the five year cure rate for Squamous Cell Carcinoma?
What is the five year cure rate for Squamous Cell Carcinoma?
Which of the following best describes Merkel Cell Carcinoma?
Which of the following best describes Merkel Cell Carcinoma?
Which factor is least likely to be associated with development of Merkel Cell Carcinoma?
Which factor is least likely to be associated with development of Merkel Cell Carcinoma?
Approximately what percentage of Merkel Cell Carcinomas have been linked to the Merkel Polyomavirus?
Approximately what percentage of Merkel Cell Carcinomas have been linked to the Merkel Polyomavirus?
Which treatment is most often regarded as the standard of care for Merkel cell carcinoma patients with Metastases?
Which treatment is most often regarded as the standard of care for Merkel cell carcinoma patients with Metastases?
Melanoma arises from which type of cells within the skin?
Melanoma arises from which type of cells within the skin?
Which characteristic is not a suspicious sign of melanoma?
Which characteristic is not a suspicious sign of melanoma?
In what percentage of cases does melanoma arise in the area of the head and neck?
In what percentage of cases does melanoma arise in the area of the head and neck?
Superficial Spreading Melanoma accounts for approximately what percentage of all melanomas?
Superficial Spreading Melanoma accounts for approximately what percentage of all melanomas?
Which clinical feature primarily distinguishes Nodular Melanoma from Superficial Spreading Melanoma?
Which clinical feature primarily distinguishes Nodular Melanoma from Superficial Spreading Melanoma?
Which of the following types of melanomas is least common?
Which of the following types of melanomas is least common?
What is the defining characteristic of Acrolentiginous Melanoma?
What is the defining characteristic of Acrolentiginous Melanoma?
According to Clark's classification, which level indicates that a tumor has invaded the reticular dermis?
According to Clark's classification, which level indicates that a tumor has invaded the reticular dermis?
According to the Breslow Classification, what depth of invasion is associated with a 25% incidence of regional metastasis?
According to the Breslow Classification, what depth of invasion is associated with a 25% incidence of regional metastasis?
For Clark's level 2-5 melanomas, what treatment approach is generally recommended?
For Clark's level 2-5 melanomas, what treatment approach is generally recommended?
What is the approximate 5-year survival rate for melanoma when the disease is confined to the primary site?
What is the approximate 5-year survival rate for melanoma when the disease is confined to the primary site?
According to the TNM staging system, which of the following is NOT a characteristic of how primary tumors are staged?
According to the TNM staging system, which of the following is NOT a characteristic of how primary tumors are staged?
What classification defines the presence of distant metastases to distant skin, subcutaneous, or lymph node sites, with a normal serum LDH?
What classification defines the presence of distant metastases to distant skin, subcutaneous, or lymph node sites, with a normal serum LDH?
Which of the following etiologic factors is LEAST associated with Squamous Cell Carcinoma?
Which of the following etiologic factors is LEAST associated with Squamous Cell Carcinoma?
A patient presents with an ulcerated lesion that appears to be arising within a burn scar that they have had for over 10 years. This presentation is MOST suggestive of what?
A patient presents with an ulcerated lesion that appears to be arising within a burn scar that they have had for over 10 years. This presentation is MOST suggestive of what?
Which of the following clinical features is most characteristic of Bowen's disease?
Which of the following clinical features is most characteristic of Bowen's disease?
If an actinically induced Squamous Cell Carcinoma is treated initially, but recurs, what is the approximate cure rate if re-treatment is administered?
If an actinically induced Squamous Cell Carcinoma is treated initially, but recurs, what is the approximate cure rate if re-treatment is administered?
Which of the following is NOT an indication for excision with frozen section pathologic diagnosis for Squamous Cell Carcinoma?
Which of the following is NOT an indication for excision with frozen section pathologic diagnosis for Squamous Cell Carcinoma?
Merkel Cell Carcinoma has which of the following characteristics?
Merkel Cell Carcinoma has which of the following characteristics?
According to the TNM staging system for melanoma, a lesion with a thickness of 1.5 mm without ulceration would be classified as:
According to the TNM staging system for melanoma, a lesion with a thickness of 1.5 mm without ulceration would be classified as:
A patient's melanoma is staged as T3b N1a M0. Which of the following statements is MOST accurate regarding this staging?
A patient's melanoma is staged as T3b N1a M0. Which of the following statements is MOST accurate regarding this staging?
A patient with melanoma demonstrates metastases only to distant skin sites with a normal serum LDH. According to the TNM staging system, this would be classified as:
A patient with melanoma demonstrates metastases only to distant skin sites with a normal serum LDH. According to the TNM staging system, this would be classified as:
What is the recommended surgical approach for a Clark's level 4 melanoma, where the depth of invasion is determined to be 2.0 mm?
What is the recommended surgical approach for a Clark's level 4 melanoma, where the depth of invasion is determined to be 2.0 mm?
A melanoma patient's disease is confined to the primary site. What is their approximate 5-year survival rate?
A melanoma patient's disease is confined to the primary site. What is their approximate 5-year survival rate?
Which of the following most accurately describes the characteristics of Acrolentiginous Melanoma?
Which of the following most accurately describes the characteristics of Acrolentiginous Melanoma?
What is the significance of ulceration in the context of melanoma staging?
What is the significance of ulceration in the context of melanoma staging?
A patient presents with a superficial melanoma that is 0.6 mm thick and Clark's level II. According to the content, which is the appropriate management?
A patient presents with a superficial melanoma that is 0.6 mm thick and Clark's level II. According to the content, which is the appropriate management?
A patient is diagnosed with Merkel Cell Carcinoma. What percentage of Merkel cell cancers have been linked to Merkel Polyomavirus?
A patient is diagnosed with Merkel Cell Carcinoma. What percentage of Merkel cell cancers have been linked to Merkel Polyomavirus?
Following a new diagnosis of Merkel Cell Carcinoma, which feature would be LEAST likely to prompt suspicion for this diagnosis?
Following a new diagnosis of Merkel Cell Carcinoma, which feature would be LEAST likely to prompt suspicion for this diagnosis?
A surgeon removes a Merkel Cell Carcinoma and determines that there is confirmed metastastic diease. What would likely be the intervention that seems to be the 'standard of care' in that circumstance?
A surgeon removes a Merkel Cell Carcinoma and determines that there is confirmed metastastic diease. What would likely be the intervention that seems to be the 'standard of care' in that circumstance?
Which of the following best describes the typical appearance of Nodular Melanoma?
Which of the following best describes the typical appearance of Nodular Melanoma?
When is prophylactic resection of lymph nodes considered for melanoma patients?
When is prophylactic resection of lymph nodes considered for melanoma patients?
What 5 year survival rate would you likely expect in a patient being treated for Melanoma where regional lymph nodes are involved?
What 5 year survival rate would you likely expect in a patient being treated for Melanoma where regional lymph nodes are involved?
Which of the following is often confused with eczema or fungal infection, clinically?
Which of the following is often confused with eczema or fungal infection, clinically?
Which of the following basal cell carcinoma variants is sometimes referred to as a rodent ulcer?
Which of the following basal cell carcinoma variants is sometimes referred to as a rodent ulcer?
What is the approximate 5-year cure rates for nodular and superficial basal cell carcinoma lesions with surgical excision with 4 to 5 mm margins?
What is the approximate 5-year cure rates for nodular and superficial basal cell carcinoma lesions with surgical excision with 4 to 5 mm margins?
Which of the following is characteristic to lesions that are less than 6 mm in diameter in high-risk sites of an excised basal cell carcinoma patient?
Which of the following is characteristic to lesions that are less than 6 mm in diameter in high-risk sites of an excised basal cell carcinoma patient?
A patient with a history of radiation therapy presents with a firm, poorly marginated ulcer. How long is it suggested lesions that are radiation induced take to develop?
A patient with a history of radiation therapy presents with a firm, poorly marginated ulcer. How long is it suggested lesions that are radiation induced take to develop?
A patient has undergone surgical excision for basal cell carcinoma. Which of the following characteristics of the lesion would suggest a lower risk of recurrence?
A patient has undergone surgical excision for basal cell carcinoma. Which of the following characteristics of the lesion would suggest a lower risk of recurrence?
Marjolin's ulcers typically exhibit which growth pattern and metastatic potential?
Marjolin's ulcers typically exhibit which growth pattern and metastatic potential?
Which of the following interventions is the recommended treatment for Bowen's disease?
Which of the following interventions is the recommended treatment for Bowen's disease?
Metastasis is more likely from what kind of squamous cell carcinoma?
Metastasis is more likely from what kind of squamous cell carcinoma?
Which factor is LEAST associated with the development of melanoma?
Which factor is LEAST associated with the development of melanoma?
What is the usual order of treatment for Marjolin's Ulcer
What is the usual order of treatment for Marjolin's Ulcer
Which of the following is NOT a suspicious sign of melanoma?
Which of the following is NOT a suspicious sign of melanoma?
A patient presents with a lesion that appears as one or more small darkly pigmented papules superimposed on a flat, light brown patch and found almost exclusively on the face. What is the likely diagnosis?
A patient presents with a lesion that appears as one or more small darkly pigmented papules superimposed on a flat, light brown patch and found almost exclusively on the face. What is the likely diagnosis?
A patient with multiple comorbidities related to immunosuppression has a skin lesion suggestive of Merkel Cell Carcinoma. This falls under the umbrella of which of the AEIOU acronym?
A patient with multiple comorbidities related to immunosuppression has a skin lesion suggestive of Merkel Cell Carcinoma. This falls under the umbrella of which of the AEIOU acronym?
After surgical excision of a cutaneous malignancy, the pathology report indicates that the tumor has invaded the reticular dermis. According to Clark's classification, this corresponds to:
After surgical excision of a cutaneous malignancy, the pathology report indicates that the tumor has invaded the reticular dermis. According to Clark's classification, this corresponds to:
Following diagnosis, which of these is most important to complete staging for melanoma?
Following diagnosis, which of these is most important to complete staging for melanoma?
What does stage II melanoma include?
What does stage II melanoma include?
A patient presents with a skin lesion that is flush with the skin, erythematous, and scaly. Which type of basal cell carcinoma (BCC) is most likely?
A patient presents with a skin lesion that is flush with the skin, erythematous, and scaly. Which type of basal cell carcinoma (BCC) is most likely?
Which of the following clinical features is most suggestive of nodular basal cell carcinoma?
Which of the following clinical features is most suggestive of nodular basal cell carcinoma?
A patient is diagnosed with a basal cell carcinoma (BCC) on their cheek. Which characteristic of the lesion would suggest a lower risk of recurrence after surgical excision?
A patient is diagnosed with a basal cell carcinoma (BCC) on their cheek. Which characteristic of the lesion would suggest a lower risk of recurrence after surgical excision?
What is a key difference in the development of squamous cell carcinoma in Marjolin's ulcer compared to radiation-induced lesions?
What is a key difference in the development of squamous cell carcinoma in Marjolin's ulcer compared to radiation-induced lesions?
Bowen's disease is characterized by which of the following?
Bowen's disease is characterized by which of the following?
How does the metastatic potential of Marjolin's ulcer typically change over time?
How does the metastatic potential of Marjolin's ulcer typically change over time?
Distant metastases in melanoma are categorized based on the location of disease involvement and which of the following?
Distant metastases in melanoma are categorized based on the location of disease involvement and which of the following?
What is the significance of ulceration in the context of melanoma staging and how does it affect the TNM classification?
What is the significance of ulceration in the context of melanoma staging and how does it affect the TNM classification?
Which of the following characteristics is most indicative of a Merkel cell carcinoma, aligning with the components of the AEIOU acronym?
Which of the following characteristics is most indicative of a Merkel cell carcinoma, aligning with the components of the AEIOU acronym?
A patient is diagnosed with Merkel cell carcinoma and has confirmed metastatic disease. What treatment approach is most often considered the standard of care?
A patient is diagnosed with Merkel cell carcinoma and has confirmed metastatic disease. What treatment approach is most often considered the standard of care?
Which of the following factors is most closely related to the development of melanoma, taking into account the predisposing factors?
Which of the following factors is most closely related to the development of melanoma, taking into account the predisposing factors?
What does Clark's classification primarily assess in the context of melanoma staging?
What does Clark's classification primarily assess in the context of melanoma staging?
When is prophylactic resection of lymph nodes considered for melanoma patients, according to the material?
When is prophylactic resection of lymph nodes considered for melanoma patients, according to the material?
Following initial treatment for an actinically induced squamous cell carcinoma, the recurrence rate is 10%. What is the expected cure rate after re-treatment?
Following initial treatment for an actinically induced squamous cell carcinoma, the recurrence rate is 10%. What is the expected cure rate after re-treatment?
In the context of staging and prognosis for Melanoma, which of the following would indicate a better prognosis? The serum LDH level is...
In the context of staging and prognosis for Melanoma, which of the following would indicate a better prognosis? The serum LDH level is...
Which of the following locations for BCC lesions less than 6 mm in diameter is associated with a low likelihood of recurrence after surgical excision?
Which of the following locations for BCC lesions less than 6 mm in diameter is associated with a low likelihood of recurrence after surgical excision?
Which of the following basal cell carcinoma variants is likely to be confused with eczema or fungal infection?
Which of the following basal cell carcinoma variants is likely to be confused with eczema or fungal infection?
Which of the following best describes the appearance of a keratoacanthoma?
Which of the following best describes the appearance of a keratoacanthoma?
Most common type of melanoma in African Americans?
Most common type of melanoma in African Americans?
Flashcards
Basal Cell Carcinoma (BCC)
Basal Cell Carcinoma (BCC)
The most common type of skin cancer, accounting for roughly 60% of all skin cancers.
Etiologic factors of BCC
Etiologic factors of BCC
Chronic sun exposure, radiation, arsenic, burns/scars, genetic disorders, and nevus sebaceous.
Superficial Basal Cell Carcinoma
Superficial Basal Cell Carcinoma
Flush with the skin, erythematous, and scaly. It may show shallow ulcers, crusting, or atrophic scarring. Can be confused with eczema or fungal infection.
Nodular Basal Cell Carcinoma
Nodular Basal Cell Carcinoma
Signup and view all the flashcards
Pigmented Basal Cell Carcinoma
Pigmented Basal Cell Carcinoma
Signup and view all the flashcards
Morpheaform/Sclerosing BCC
Morpheaform/Sclerosing BCC
Signup and view all the flashcards
Merkel Cell Carcinoma
Merkel Cell Carcinoma
Signup and view all the flashcards
Adnexal Carcinoma
Adnexal Carcinoma
Signup and view all the flashcards
PTCH1
PTCH1
Signup and view all the flashcards
Marjolin's Ulcer
Marjolin's Ulcer
Signup and view all the flashcards
Radiation-Induced Cancer
Radiation-Induced Cancer
Signup and view all the flashcards
Bowen's Disease
Bowen's Disease
Signup and view all the flashcards
Melanoma
Melanoma
Signup and view all the flashcards
Superficial Spreading melanoma
Superficial Spreading melanoma
Signup and view all the flashcards
Nodular Melanoma
Nodular Melanoma
Signup and view all the flashcards
Lentigo Maligna Melanoma
Lentigo Maligna Melanoma
Signup and view all the flashcards
Acrolentiginous Melanoma
Acrolentiginous Melanoma
Signup and view all the flashcards
Study Notes
Malignant Diseases of the Skin
- Basal cell carcinoma makes up roughly 60% of skin cancers.
Etiologic Factors for Basal Cell Carcinoma
- Chronic sun exposure
- Radiation
- Arsenic
- Burns and scars
- Genetic disorders such as xeroderma pigmentosa, basal cell nevus syndrome, and albinism
- Nevus sebaceous, present at birth on the scalp or face, has approximately 10% chance of becoming BCC
Common Clinical Presentations of Basal Cell Carcinoma
- Superficial Basal Cell Carcinoma (30%) presents with skin flush, is erythematous and scaly, with or without shallow ulcers or crusting, and atrophic scarring, is often confused with eczema or fungal infection
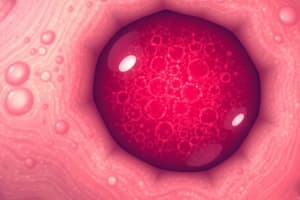
- Nodular Basal Cell Carcinoma (60%) present as a flesh-colored nodule featuring telangiectatic vessels, and larger lesions form a peripheral rolled border, also known as a "rodent ulcer"
- Pigmented Basal Cell Carcinoma is distinguished by its brown pigmentation, and is otherwise similar to nodular BCC
- Morpheafarm or Sclerosing Basal Cell Carcinoma (5-10%) presents as a firm white or yellowish plaque with an ill-defined border
- Induration is always present.
- Ulceration rarely occurs.
- Patients frequently describe the presentation as an "enlarging scar".
- Merkel Cell Carcinoma is a relatively new entity that resembles BCC histologically and commonly occurs as a single tumor in elderly individuals
- Adnexal carcinoma arises from sebaceous sweat glands
Basal Cell Carcinoma Recurrence
- Lesions with a low likelihood of recurrence are less than 6 mm in diameter in high-risk areas like the central face, nose, lips, eyelids, eyebrows, periorbital skin, chin, mandible, ears, preauricular and postauricular areas, temples, hands and feet
- Lesions with a low likelihood of recurrence are less than 10 mm in diameter in other areas of the head and neck or less than 20 mm in diameter anywhere excluding hands and feet
- Nodular or superficial histopathologic growth patterns have low likelihood of recurrence
- Well-defined clinical borders have low likelihood of recurrence
- 40% of patients with one BCC will develop another lesion within 5 years
- Surgical excision with 4 to 5 mm margins has a five year cure rate exceeding 95%
- Surgical excision is used for lesions with low and high risk of recurrence
- Electrodesiccation and curettage (ED&C) is most appropriate for low-risk superficial or nodular BCCs on the trunk or extremities
- BCCs occurring in low-risk sites have a three percent recurrence rate
- BCCs less than 6 mm in diameter in high-risk sites have a 5 percent failure rate
- Tumors greater than 6 mm have a recurrence rate of 18 percent
Molecular Pathogenesis of Basal Cell Carcinoma
- PTCH1 is a tumor suppressor gene on chromosome 9
- Similar to retinoblastoma's "two hit" hypothesis
- Two hits to the same cell are needed for sporadic cases
- One somatic hit plus inheritance of a defective allele is needed for familial cases of basal cell nevus syndrome or xeroderma pigmentosum)
- PTCH proteins, along with SMO, are receptors for the hedgehog (HH) protein that activates the Sonic Hedgehog signaling pathway
- PTCH-induced repression of SMO limits the effects of the SHH signal
- Inactivating mutations of the PTCH gene lead to overexpression of the SHH signal
- P53 mutations are less frequent in BCCs than cutaneous squamous cell cancers
Squamous Cell Carcinoma
- Squamous cell carcinoma represents roughly 30% of all skin cancers.
Etiologic Factors
- Radiation injury
- Chronic sun exposure
- Chronic chemical exposure (hydrocarbons, arsenic)
- Burns
- Unstable scars, such as Marjolin's ulcer
- Actinic Keratosis
- Leukoplakia
- Chronic ulcers
- Chronic draining sinus tracts
Clinical Presentation
- Common sites include ears, lips, temples, upper face, and dorsum of hands
- Early tumors appear like actinic keratosis except scaling is raised in a skin-colored papule
- Advanced lesions may ulcerate, presenting a horny and crusted appearance
- Nodular Squamous Cell Carcinoma is a dome-shaped, skin-colored papule that is usually ulcerated
- These appear to grow outward, a hemispherical shape with sharp margins
- May or may not occur on sun-damaged skin
- Most commonly located on the lower lips, ears, and dorsum of hands.
- Keratoacanthoma
- Is rapidly growing
- Features a tendency for spontaneous resolution
- Has a histological and clinical appearance similar to nodular squamous cell carcinoma
Marjolin's Ulcer
- Chronic unstable burn scars or chronic draining osteomyelitis can cause premalignant changes leading to squamous cell carcinoma
- Present on the margins of ulcers for 5 or more years
- Typically slow-growing, but tend to recur and metastasize rapidly after resection
- Treatment entails wide local excision followed by regional node dissection two to four weeks after the wound has healed
Radiation-Induced Malignancy
- Occurs as a firm, poorly marginated ulcer at previously radiated sites
- Lesions are very slow to develop over 15 or more years after radiation
Bowen's Disease:
- Presents with a characteristic appearance of a slowly growing, erythematous patch with fine scaling and small crusted areas
- Characteristics
- A fairly sharp, irregular outer border.
- The color varies from red to tan.
- Surgical excision is the recommended treatment.
Squamous Cell Carcinoma Pathogenesis
- SCC appears from moderately well-differentiated epithelial cells
- Low grade SCC shows evidence of keratinization and has few mitotic figures per high powered field
- More aggressive lesions display increased keratinization and have increased mitotic rate
Squamous Cell Carcinoma Course and Prognosis
- Untreated squamous cell carcinoma will invade and destroy skin much more aggressively than basal cell carcinoma
- Actinic induced squamous cell carcinomas display a less than 1-2% metastatic rate
- Nodular squamous cell carcinomas display an approximate 10% rate
- Keratoacanthomas usually do not metastasize
- Recurrence occurs 10% of the time following initial treatment, but re-treatment leads to a 98% cure rate.
- Five year cure rates for SCC range from 90-95%.
Current Squamous Cell Carcinoma Treatments
- Treatment options for small (less than 2 cm) actinically induced squamous cell carcinomas include same modalities as basal cell carcinomas
- More aggressive, larger lesions, excision with frozen section pathologic diagnosis is preferred
New Treatment Concepts
- Imiquimod™
- Matristem™
- ACeLL™
Basal Cell Varients
- Merkel Cell Cancer demonstrates rising interest and incidence
- Journal American Medical Association, July 3, 2018, volume 320, #1, pages 18-20
- Rare, but on the rise
- 80% of Merkel cell cancers are due to Merkel polyomavirus while 20% are due to UV exposure
- More aggressive than melanoma
- Merkel Cell Tumor, AEIOU, significant acronym
- A - Asymptomatic
- E - Expanding rapidly
- I - Immunosuppressive
- O - Older patients, usually over 70 years of age
- U - UV exposure
- 90% of Merkel cell carcinomas have three or more of these features
Merkel Cell Treatment
- Excisional surgery, possible sentinel node
- Radiotherapy
- Immunotherapy has shown promise
- Avelumab appears to be the standard of care for all metastatic Merkel cell patients
Melanoma
- Arises from melanocytes, the pigment producing cells of the skin
Melanoma: Suspicious Signs
- Irregular borders
- Variegated color (red, white, blue shades)
- Increase in size, or change in color.
- Scaliness, erosion, oozing, crusting, bleeding, or development of satellite lesions
Melanoma Epidemiology
- Represents 1% of all cancers
- 20-30% arise in the head and neck area
- Occurs predominantly in caucasian patients
- Patients between the ages of 30 and 60 are commonly affected
- Approximately 50% of malignant melanomas are from junctional or compound nevi, and 50% arise anew
- 14,000 new cases are diagnosed yearly in the U.S.
Melanoma Clinical Presentations
-
Superficial spreading melanoma: 70% of melanomas
- Presents as a relatively flat topped, slow growing pigmented papule or plaque
- Characterized by Irregular borders, irregular pigmentation and black, red, white, or blue color
- Lesion is frequently wider than it is tall and larger lesions can appear bumpy or lobulated, and may spread pigmentation to adjacent tissue
- In men, the back is the most common occurence, while in women, occurence is most common on the legs
-
Nodular Melanoma, 15% of melanomas
- Appears as dome shaped, darkly pigmented papules or nodules
- Grows faster and develops a deeper color than the superficial spreading type
- More evenly pigmented, usually as tall as they are wide
-
Lentigo Maligna Melanoma is the least common type
- Found almost exclusively on the face
- Arises from pre-existing lentigo, apperaing as one or more small, darkly pigmented papules on a flat, light brown patch, called "Hutchinsons' freckle"
-
Acrolentiginous Melanoma, accounts for 10% of melanomas
- Most common type of melanoma occurs on digits, palms, and soles, and most often among African Americans
- One or more dark smooth papules stand against a background of gray or black macular with uneven pigmentation
Melanoma: Predisposing Factors
- Sun exposure, more closely tied to number and severity of individual sunburns, rather than lifetime sun exposure
- Ten percent of patients have positive family histories relating to genetics
- Patients with congenital hairy nevi are at higher risk for malignant transformation and these have a 15-40 percent incidence.
- Patients with compromised Inate or iatrogenic immune systems also increase risk
Melanoma: Staging and Diagnosis
- Clark's classification assess level of invasion
- Level 1: Tumor confined to the epidermis
- Level 2: Tumor invades papillary dermis
- Level 3: Tumor fills papillary dermis, but not reticular dermis
- Level 4: Tumor invades reticular dermis
- Level 5: Tumor invades subcutaneous fat
- Breslow Classification, measures depth of invasion in millimeters, correlating with the incidence of regional metastasis
- Lesions up to 0.75 mm depth have 0% incidence of regional metastasis
- Lesions measuring 0.76-1.5 mm depth have a 25% incidence of regional metastasis
- Lesions between 1.51 and 3.99 mm depth have a 51% incidence of regional metastasis -Lesions greater than 4.0 mm have a 62% incidence of regional metastasis.
- To complete the staging, patients must have a thorough history and physical review as well as a complete blood count with SMA-12, urinalysis, and chest X-ray
Melanoma: Metastases
- Melanoma can metastasize through the lymphatic system and bloodstream to any organ of the body
- Patients with Clark's level 1, 2 or 3 lesions and a depth less than 0.76 mml are at low risk of metastasis
- Patients with Clark's level 4 or 5 lesions and a depth over 1.5 mm are at high risk of metastasis
Melanoma Treatment
- Determined by the depth of invasion and tumor level
- Excision is required for Clark's level 1 Lesions
- Only a cuff of normal tissue is required (usually .5-1c mm margins)
- Excision is required for Clark's level 2-5
- A wide margin and underlying fascia is required, unless Lesions occur on the face where lesser margins are adequate
Melanoma treatment: Node Resection
- Clinically involved regional lymph nodes with Clark's level 2-5 lesions should be retreated
- Prophylactic resection of lymph nodes: controversial among experts, though some say that it can be performed on patients with level 5 disease or if a tumor overlies a lymph node area.
- Lymph node resection is recommended if the depth of the lesion is greater than 0.75mm or Clark's level 3.
- It is intended to aid in staging and enhance survival
Melanoma Adjuvent Therapy
- A. Regional hyperthermic perfusion involves isolating the blood supply of a limb with a pump/oxygenator, enabling high doses of chemotherapy at elevated temperatures of to be delivered to the limb without side effects of systemic toxicity
- B. Chemotherapy has been found to significantly alter the course of disease
- C. Immunotherapy is useful to control cutaneous metastases
- However is not effective against visceral metastases
- D. Radiotherapy is strictly palliative and is used for brain and bone metastases
Melanoma Prognosis
- If the disease is confined to the primary site, a five year survival rate approaches 80-90%
- If regional lymph nodes are involved, the five year survival rate drops to 30-50%
- Patients with distant or visceral metastases usually live no more than 12 months
Melanoma Staging
-
Tumor thickness, ulceration, and mitotic rate are key qualities to note when staging Melanoma
-
Primary Tumor (T): tumor thickness, ulceration and mitotic rate
- T1: ≤1mm
- T2: 1.01 to 2 mm
- T3: 2.01 to 4 mm
- T4: >4 mm
- "a" or "b" note the presence or abcense of ulcerations
-
10-year survival decreases with progressively increased tumor thickness
- Decreases from 96 percent for primary lesions less than 0.5 mm to 54 percent for lesions measuring 4.01 to 6 mm thick
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.