Podcast
Questions and Answers
What are A-B toxins primarily composed of?
What are A-B toxins primarily composed of?
- One polypeptide part
- Four polypeptide parts
- Three polypeptide parts
- Two polypeptide parts (correct)
What is a characteristic effect of endotoxins on the human body?
What is a characteristic effect of endotoxins on the human body?
- Lead to increased capillary permeability (correct)
- Stimulate an immediate immune response
- Cause only localized symptoms
- Induce effective antitoxin formation
What role do plasmids play in bacterial pathogenicity?
What role do plasmids play in bacterial pathogenicity?
- They are involved in cellular respiration
- They eliminate immune responses from hosts
- They can carry genes for virulence factors (correct)
- They require a host to replicate
How do superantigens affect the immune system?
How do superantigens affect the immune system?
Which type of toxin is produced by bacteria to lyse host cells by disrupting their plasma membranes?
Which type of toxin is produced by bacteria to lyse host cells by disrupting their plasma membranes?
What is one mechanism by which viruses evade the host's immune defenses?
What is one mechanism by which viruses evade the host's immune defenses?
What common symptom is associated with exposure to endotoxins?
What common symptom is associated with exposure to endotoxins?
What characterizes the intracellular growth of viruses?
What characterizes the intracellular growth of viruses?
What do infected cells produce to protect neighboring uninfected cells from viruses?
What do infected cells produce to protect neighboring uninfected cells from viruses?
Which mechanism is commonly employed by fungi to evade host defenses?
Which mechanism is commonly employed by fungi to evade host defenses?
What effect do trichothecenes produced by certain fungi have on the host?
What effect do trichothecenes produced by certain fungi have on the host?
What is a characteristic pathogenic mechanism of protozoa?
What is a characteristic pathogenic mechanism of protozoa?
What is a consequence of the resistance to antifungal drugs in pathogenic fungi?
What is a consequence of the resistance to antifungal drugs in pathogenic fungi?
Which protozoan is known to prevent normal digestion within macrophages?
Which protozoan is known to prevent normal digestion within macrophages?
What is one of the mechanisms viruses employ to evade interferon responses?
What is one of the mechanisms viruses employ to evade interferon responses?
What disease is caused by ergotism produced from Claviceps purpurea?
What disease is caused by ergotism produced from Claviceps purpurea?
Which bacterial pathogen requires low pH for replication within phagocytes?
Which bacterial pathogen requires low pH for replication within phagocytes?
How do biofilms enhance resistance to phagocytosis?
How do biofilms enhance resistance to phagocytosis?
What is the primary function of siderophores in pathogenic bacteria?
What is the primary function of siderophores in pathogenic bacteria?
Which of the following is NOT a mechanism by which microorganisms can damage host cells?
Which of the following is NOT a mechanism by which microorganisms can damage host cells?
Which pathogen can escape or inhibit phagosome-lysosome fusion?
Which pathogen can escape or inhibit phagosome-lysosome fusion?
What role does the extracellular polymeric substance (EPS) play in biofilms?
What role does the extracellular polymeric substance (EPS) play in biofilms?
How do some pathogens directly acquire iron without using siderophores?
How do some pathogens directly acquire iron without using siderophores?
What happens to phagocytes when they interact with the EPS of Pseudomonas aeruginosa?
What happens to phagocytes when they interact with the EPS of Pseudomonas aeruginosa?
Which molecule is found in Streptococcus pyogenes and aids in attachment while resisting phagocytosis?
Which molecule is found in Streptococcus pyogenes and aids in attachment while resisting phagocytosis?
What role does Opa Protein play in Neisseria gonorrhoeae?
What role does Opa Protein play in Neisseria gonorrhoeae?
Which enzyme produced by bacteria helps to form clots that protect them from phagocytosis?
Which enzyme produced by bacteria helps to form clots that protect them from phagocytosis?
Which extracellular enzyme helps to spread infections like gas gangrene by breaking down collagen?
Which extracellular enzyme helps to spread infections like gas gangrene by breaking down collagen?
What does the presence of mycolic acid in Mycobacterium tuberculosis help the bacterium achieve?
What does the presence of mycolic acid in Mycobacterium tuberculosis help the bacterium achieve?
Which bacterial function is triggered by adhesins leading to membrane ruffling in host cells?
Which bacterial function is triggered by adhesins leading to membrane ruffling in host cells?
Which bacteria use invasins to rearrange actin filaments in host cells?
Which bacteria use invasins to rearrange actin filaments in host cells?
What is the primary function of kinases produced by bacteria?
What is the primary function of kinases produced by bacteria?
How does HIV evade the immune system?
How does HIV evade the immune system?
What is a direct outcome of cytopathic effects caused by viral infections?
What is a direct outcome of cytopathic effects caused by viral infections?
Which type of cytopathic effect directly results in cell death?
Which type of cytopathic effect directly results in cell death?
What occurs during the inclusion bodies formation cytopathic effect?
What occurs during the inclusion bodies formation cytopathic effect?
Which cytopathic effect is characterized by the formation of large multinucleate cells?
Which cytopathic effect is characterized by the formation of large multinucleate cells?
Which effect could lead to cancer due to viral infection?
Which effect could lead to cancer due to viral infection?
What is a potential effect of the measles virus on the immune response?
What is a potential effect of the measles virus on the immune response?
Which of the following describes how viral proteins can affect host cells?
Which of the following describes how viral proteins can affect host cells?
Flashcards are hidden until you start studying
Study Notes
Bacterial Encapsulation
- Encapsulation enhances virulence by preventing phagocytosis and complement activation
- Examples of encapsulated bacteria include: Klebsiella pneumoniae, Haemophilus influenzae, Bacillus anthracis, and Yersinia pestis
Bacterial Cell Wall Components
- M Protein (found in Streptococcus pyogenes) aids in attachment and resists phagocytosis
- Opa Protein (present in Neisseria gonorrhoeae) facilitates attachment and entry into host cells
- Mycolic Acid (in Mycobacterium tuberculosis) helps resist digestion by phagocytes
Bacterial Exoenzymes
- Coagulases convert fibrinogen to fibrin, forming protective clots
- Kinases (like streptokinase) break down fibrin clots
- Hyaluronidase hydrolyzes hyaluronic acid, aiding tissue spread
- Collagenase breaks down collagen, facilitating spread of infections like gas gangrene
- Some bacteria produce IgA proteases to destroy IgA antibodies, aiding adherence
Bacterial Penetration of Host
- Pathogens attach using adhesins, triggering host cell signals for entry
- Bacteria like Salmonella and E. coli use invasins to rearrange actin filaments in host cells, leading to membrane ruffling and engulfment
- Once inside, some bacteria like Shigella and Listeria can use actin for movement
Bacterial Survival Inside Phagocytes
- Coxiella burnetii requires low pH for replication within phagocytes
- Some bacteria escape or inhibit phagosome-lysosome fusion (Mycobacterium tuberculosis, HIV)
Bacterial Biofilms
- Biofilms enhance resistance to phagocytosis
- Phagocytes struggle to penetrate the extracellular polymeric substance (EPS)
- EPS shields bacterial antigens from immune recognition and can even kill phagocytes (Pseudomonas aeruginosa)
Bacterial Iron Requirements
- Most pathogenic bacteria require iron for growth
- Free iron levels in the human body are low
- Siderophores are proteins secreted by bacteria to bind and sequester iron from host iron-transport proteins (e.g., transferrin, lactoferrin).
- The iron-siderophore complex is taken up by bacterial receptors, allowing bacteria to acquire essential iron
Damage Mechanisms of Microorganisms
- Using the host's nutrients
- Causing direct damage at the site of invasion
- Producing toxins that affect distant sites
- Inducing hypersensitivity reactions
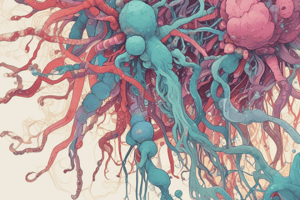
Exotoxin Types
- A-B Toxins: Composed of two polypeptide parts (A for activity, B for binding). Example: diphtheria toxin
- Membrane-Disrupting Toxins: Lyse host cells by disrupting plasma membranes; examples include leukocidins and hemolysins
- Superantigens: Stimulate excessive immune responses by activating T cells nonspecifically, leading to severe symptoms like shock
Endotoxin Effects
- Common symptoms include chills, fever, weakness, and potentially septic shock due to increased capillary permeability and fluid loss
- Endotoxins do not promote effective antitoxin formation
Plasmids and Pathogenicity
- Plasmids carry genes for virulence factors (e.g., toxins, adhesins)
- Lysogeny: Some bacteriophages integrate their DNA into bacterial genomes, leading to new pathogenic traits in lysogenic bacteria
Pathogenic Properties of Viruses
- Access to Host: Viruses must gain entry into a host organism.
- Evasion of Immune Defenses: Successful viruses evade the host's immune system.
- Cell Damage: Viruses cause damage or death to host cells while replicating
Viral Mechanisms for Evading Host Defenses
- Intracellular Growth: Viruses can replicate inside host cells, inaccessible to immune components
- Attachment Sites: Viruses possess specific sites that bind to receptors on target cells, facilitating entry (Example: Rabies virus mimics acetylcholine to enter cells)
- HIV Evasion: Hides attachment sites from immune detection, targets CD4 proteins on T lymphocytes, making it difficult for antibodies to neutralize the virus
Cytopathic Effects (CPE) of Viruses
- Cell Death: Viral infections typically lead to host cell death via: Accumulation of viruses, Disruption of cellular functions (e.g., DNA/RNA/protein synthesis)
- Types of CPE: Cytocidal Effects (directly result in cell death), Noncytocidal Effects (cause damage without killing the cell)
Specific Cytopathic Effects of Viruses
- Inhibition of Macromolecular Synthesis: Some viruses halt cellular processes (e.g., Simplexvirus stops mitosis)
- Lysosomal Enzyme Release: Host cell lysosomes release enzymes, leading to cell destruction
- Inclusion Bodies Formation: Viral components aggregate in infected cells, aiding in diagnosis (e.g., Negri bodies in rabies)
- Syncytium Formation: Infected cells may fuse to form large multinucleate cells seen in measles and mumps
- Functional Changes Without Visible Damage: Example includes measles virus reducing IL-12 production, impairing immune response
- Antigenic Changes on Cell Surfaces: Viral proteins alter host cell antigens, prompting immune targeting
- Chromosomal Damage: Some viruses induce chromosomal breakage or activate oncogenes, leading to cancer risks
- Cell Transformation: Certain viruses can transform host cells into abnormal growth patterns, losing contact inhibition
Interferon Production
- Infected cells produce alpha and beta interferons to protect neighboring uninfected cells: Inhibit viral and host protein synthesis, Induce apoptosis in infected cells
- Many viruses have evolved mechanisms to evade interferon responses
Pathogenic Properties of Fungi, Protozoa, Helminths, and Algae
- Toxins: Trichothecenes (inhibit protein synthesis, cause headaches, chills, nausea), Ergotism (caused by Claviceps purpurea, leading to hallucinations and gangrene)
- Virulence Factors: Proteases for attachment, capsule production (Cryptococcus neoformans), resistance to antifungal drugs
- General Characteristics: Protozoa can cause disease through their presence and metabolic waste products
- Cell Invasion: Plasmodium invades red blood cells, Toxoplasma prevents normal digestion within macrophages, Giardia intestinalis attaches to host cells and digests tissue fluids
- Evasion of Host Defenses: Some protozoa use antigenic variation to evade the immune system (Trypanosoma)
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.