Podcast
Questions and Answers
Which statement best describes the selectivity of flucytosine in treating fungal infections?
Which statement best describes the selectivity of flucytosine in treating fungal infections?
- Flucytosine directly destroys human cells.
- Flucytosine is less toxic to humans compared to fungi due to limited conversion. (correct)
- Flucytosine has a high conversion rate in human cells.
- Flucytosine is equally toxic to both human and fungal cells.
What is the main mechanism by which azole antifungal agents exert their effects?
What is the main mechanism by which azole antifungal agents exert their effects?
- Blocking the replication of fungal DNA through direct interference.
- Activation of human immune response against fungi.
- Inhibition of cell wall synthesis in fungi.
- Disruption of fungal cell membrane by impairing ergosterol synthesis. (correct)
Which adverse effect is not typically associated with the use of flucytosine?
Which adverse effect is not typically associated with the use of flucytosine?
- Gastrointestinal ulceration (correct)
- Bone marrow toxicity
- Hepatitis (rarely)
- Alopecia
What is the significance of combining Ampho B with flucytosine?
What is the significance of combining Ampho B with flucytosine?
Which of the following azole antifungal agents falls under the imidazole group?
Which of the following azole antifungal agents falls under the imidazole group?
Which antifungal agent is primarily used for systemic candidiasis and cryptococcal meningitis?
Which antifungal agent is primarily used for systemic candidiasis and cryptococcal meningitis?
What is a common adverse effect associated with ketoconazole?
What is a common adverse effect associated with ketoconazole?
Which of the following statements about ketoconazole is true?
Which of the following statements about ketoconazole is true?
Which antifungal agent is contraindicated with amphotericin B?
Which antifungal agent is contraindicated with amphotericin B?
What is the primary route of administration for itraconazole in systemic fungal infections?
What is the primary route of administration for itraconazole in systemic fungal infections?
Which antifungal is known for causing transient visual disturbances?
Which antifungal is known for causing transient visual disturbances?
Which characteristic is true regarding fluconazole's pharmacodynamics?
Which characteristic is true regarding fluconazole's pharmacodynamics?
Which antifungal is classified as an imidazole and is primarily used topically?
Which antifungal is classified as an imidazole and is primarily used topically?
Which of the following antifungal drugs primarily disrupts the function of the cell membrane?
Which of the following antifungal drugs primarily disrupts the function of the cell membrane?
What is the primary mechanism of action for Terbinafine?
What is the primary mechanism of action for Terbinafine?
Which drug class does Griseofulvin belong to and what is its primary action?
Which drug class does Griseofulvin belong to and what is its primary action?
What is the common adverse effect associated with Amphotericin B?
What is the common adverse effect associated with Amphotericin B?
Which antifungal is known for its extensive use in systemic mycosis?
Which antifungal is known for its extensive use in systemic mycosis?
Caspofungin primarily inhibits which process in fungi?
Caspofungin primarily inhibits which process in fungi?
What distinguishes Flucytosine from other antifungal agents?
What distinguishes Flucytosine from other antifungal agents?
Which of the following correctly describes the pharmacokinetics of Amphotericin B?
Which of the following correctly describes the pharmacokinetics of Amphotericin B?
What is the main source of Amphotericin B?
What is the main source of Amphotericin B?
Nystatin is primarily used for what type of infections?
Nystatin is primarily used for what type of infections?
Inhibition of which component is crucial for the function of Azole antifungals?
Inhibition of which component is crucial for the function of Azole antifungals?
Which characteristic makes antifungal drugs more toxic compared to antibacterial drugs?
Which characteristic makes antifungal drugs more toxic compared to antibacterial drugs?
Which antifungal is typically used for treating life-threatening mycotic infections?
Which antifungal is typically used for treating life-threatening mycotic infections?
Which type of fungal infection affects the deepest layers of tissue?
Which type of fungal infection affects the deepest layers of tissue?
What is the primary mechanism of action for fluconazole?
What is the primary mechanism of action for fluconazole?
Which of these statements is true regarding Voriconazole?
Which of these statements is true regarding Voriconazole?
What type of drug interaction is associated with Itraconazole?
What type of drug interaction is associated with Itraconazole?
Which of the following statements about Echinocandins is false?
Which of the following statements about Echinocandins is false?
What is a key characteristic of Terbinafine?
What is a key characteristic of Terbinafine?
What best describes the absorption of Posaconazole?
What best describes the absorption of Posaconazole?
Which antifungal is primarily used for long-term therapy of dermatophyte infections of hair and nails?
Which antifungal is primarily used for long-term therapy of dermatophyte infections of hair and nails?
Which type of resistance is more commonly observed in severely ill or immunocompromised patients?
Which type of resistance is more commonly observed in severely ill or immunocompromised patients?
Which of the following antifungals inhibits the synthesis of fungal cell walls?
Which of the following antifungals inhibits the synthesis of fungal cell walls?
What is the primary enzyme targeted by Terbinafine?
What is the primary enzyme targeted by Terbinafine?
What makes Itraconazole effective in treating infections caused by molds?
What makes Itraconazole effective in treating infections caused by molds?
Which of the following correctly describes the pharmacokinetics of Fluconazole?
Which of the following correctly describes the pharmacokinetics of Fluconazole?
What type of infections is Caspofungin primarily indicated for?
What type of infections is Caspofungin primarily indicated for?
Flashcards
5-FU's mechanism of action
5-FU's mechanism of action
5-FU inhibits the synthesis of nucleic acids (DNA and RNA) in fungi, disrupting their growth.
Flucytosine's selectivity
Flucytosine's selectivity
Human cells are less efficient at converting flucytosine to 5-FU, making it less toxic to humans than fungi.
Azole antifungals' mechanism
Azole antifungals' mechanism
Azole antifungals target a specific enzyme in fungal cell membranes, disrupting ergosterol synthesis which weakens the cell membrane.
Groups of azole antifungals
Groups of azole antifungals
Signup and view all the flashcards
Absorption of Azole drugs
Absorption of Azole drugs
Signup and view all the flashcards
Antifungal Drugs
Antifungal Drugs
Signup and view all the flashcards
Why are antifungal drugs more toxic than antibacterial drugs?
Why are antifungal drugs more toxic than antibacterial drugs?
Signup and view all the flashcards
What is the fungal cell wall composed of?
What is the fungal cell wall composed of?
Signup and view all the flashcards
What is ergosterol?
What is ergosterol?
Signup and view all the flashcards
What do Polyene antifungal drugs do?
What do Polyene antifungal drugs do?
Signup and view all the flashcards
What is Amphotericin B?
What is Amphotericin B?
Signup and view all the flashcards
What is Amphotericin B's acute reaction?
What is Amphotericin B's acute reaction?
Signup and view all the flashcards
What do Azole antifungal drugs do?
What do Azole antifungal drugs do?
Signup and view all the flashcards
What is Fluconazole?
What is Fluconazole?
Signup and view all the flashcards
What do Allylamines antifungal drugs do?
What do Allylamines antifungal drugs do?
Signup and view all the flashcards
What is Terbinafine?
What is Terbinafine?
Signup and view all the flashcards
What do Echinocandins antifungal drugs do?
What do Echinocandins antifungal drugs do?
Signup and view all the flashcards
What is Caspofungin?
What is Caspofungin?
Signup and view all the flashcards
What is Flucytosine?
What is Flucytosine?
Signup and view all the flashcards
What kind of drug is Flucytosine?
What kind of drug is Flucytosine?
Signup and view all the flashcards
Systemic imidazoles
Systemic imidazoles
Signup and view all the flashcards
Triazole antifungals' role
Triazole antifungals' role
Signup and view all the flashcards
Adverse effect of azoles
Adverse effect of azoles
Signup and view all the flashcards
Ketoconazole antiandrogenic effect
Ketoconazole antiandrogenic effect
Signup and view all the flashcards
Ketoconazole absorption
Ketoconazole absorption
Signup and view all the flashcards
Ketoconazole half-life
Ketoconazole half-life
Signup and view all the flashcards
Ketoconazole spectrum of activity
Ketoconazole spectrum of activity
Signup and view all the flashcards
Ketoconazole clinical uses
Ketoconazole clinical uses
Signup and view all the flashcards
Fluconazole: Key Features
Fluconazole: Key Features
Signup and view all the flashcards
Fluconazole: Resistance Patterns
Fluconazole: Resistance Patterns
Signup and view all the flashcards
Fluconazole: Acquired Resistance
Fluconazole: Acquired Resistance
Signup and view all the flashcards
Itraconazole: Broad Spectrum Triazole
Itraconazole: Broad Spectrum Triazole
Signup and view all the flashcards
Voriconazole: Second-Generation Triazole
Voriconazole: Second-Generation Triazole
Signup and view all the flashcards
Posaconazole: Newest Triazole
Posaconazole: Newest Triazole
Signup and view all the flashcards
Topical Azoles: Treatment of Superficial Infections
Topical Azoles: Treatment of Superficial Infections
Signup and view all the flashcards
Terbinafine: Mechanism of Action
Terbinafine: Mechanism of Action
Signup and view all the flashcards
Echinocandins: Mechanism of Action
Echinocandins: Mechanism of Action
Signup and view all the flashcards
Griseofulvin: Microtubule Inhibitor
Griseofulvin: Microtubule Inhibitor
Signup and view all the flashcards
Dermatophytes: Common Skin Infections
Dermatophytes: Common Skin Infections
Signup and view all the flashcards
Candida albicans: A Common Yeast
Candida albicans: A Common Yeast
Signup and view all the flashcards
Aspergillus: Mold Infections
Aspergillus: Mold Infections
Signup and view all the flashcards
Cryptococcus neoformans: Yeast Infection
Cryptococcus neoformans: Yeast Infection
Signup and view all the flashcards
Zygomycetes: Serious Fungal Infections
Zygomycetes: Serious Fungal Infections
Signup and view all the flashcards
Study Notes
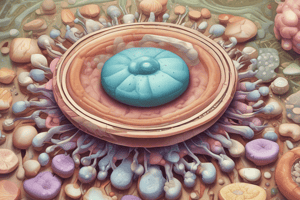
Antifungal Drugs Classification
- Antifungal drugs target superficial, cutaneous, subcutaneous, and systemic fungal infections.
- Fungi are eukaryotes, meaning antifungal drugs are more toxic than antibacterial drugs.
- Fungal cell walls contain chitin and polysaccharides, while human cell membranes contain ergosterol.
Sites of Antifungal Activity
- Membrane function: Drugs like Amphotericin B
- Ergosterol synthesis: Fluconazole, Itraconazole, Voriconazole, Naftifine, Terbinafine
- Nucleic acid synthesis: 5-Fluorocytosine
- Cell wall synthesis: Caspofungin
- Cell membrane permeability: Azoles, Polyenes, Terbinafine
- Microtubule function: Griseofulvin
Classifications Based on Mechanism of Action
- Fungal cell wall synthesis inhibitors (Echinocandins): Caspofungin
- Ergosterol binding: Amphotericin B, Nystatin
- Ergosterol/Lanosterol synthesis inhibitors: Terbinafine, Naftifine, Butenafine
- Ergosterol synthesis inhibitors: Azoles
- Nucleic acid synthesis inhibitors: 5-Fluorocytosine
- Fungal mitosis inhibitors: Griseofulvin
- Miscellaneous: Ciclopirox, Tolnaftate, Haloprogin, Undecylenic acid, Topical azoles
Classifications Based on Structure
- Antibiotics: Polyenes (e.g., Amphotericin, Nystatin, Hamycin), Heterocyclic (e.g., Benzofuran, Griseofulvin), Antimetabolite (e.g., Flucytosine), Azoles (e.g., Fluconazole, Miconazole)
Additional Information from the Text
- Specific drugs are listed within each category (e.g., Imidazoles - Ketoconazole, Clotrimazole).
- Antifungal drug uses, mechanisms, and adverse effects are detailed in further sections.
- Detailed information on specific drug classes and individual drugs is also covered.
- The text discusses the classification of antifungal drugs based on their structure, mechanism of action, and therapeutic uses.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.