Podcast
Questions and Answers
What is the primary effect of Propofol during short procedures?
What is the primary effect of Propofol during short procedures?
- Increases heart rate and blood pressure
- Enhances the effect of neuromuscular blockers
- Causes prolonged respiratory support
- Decreases heart rate and blood pressure (correct)
Which drug is primarily used for its amnesia effect during procedures?
Which drug is primarily used for its amnesia effect during procedures?
- Etomidate
- Midazolam (correct)
- Ketamine
- Fentanyl
What is a significant adverse reaction of using Fentanyl?
What is a significant adverse reaction of using Fentanyl?
- Hypertension
- Respiratory depression (correct)
- Increased gastrointestinal activity
- Increased heart rate
What is a common side effect of long-term use of Continuous Sedation agents like Propofol?
What is a common side effect of long-term use of Continuous Sedation agents like Propofol?
Which neuromuscular blocking agent has a rapid onset and short duration of action?
Which neuromuscular blocking agent has a rapid onset and short duration of action?
What is the role of Naloxone in opioid administration?
What is the role of Naloxone in opioid administration?
What is an important consideration when administering Midazolam in patients with low blood pressure?
What is an important consideration when administering Midazolam in patients with low blood pressure?
What effect does Ketamine have on blood pressure and heart rate?
What effect does Ketamine have on blood pressure and heart rate?
What adverse reaction is associated with the use of Meperidine?
What adverse reaction is associated with the use of Meperidine?
What is a key characteristic of Digoxin in treating A-Fib?
What is a key characteristic of Digoxin in treating A-Fib?
Flashcards are hidden until you start studying
Study Notes
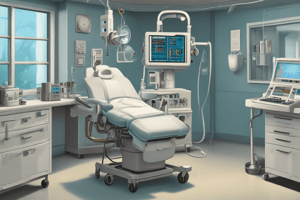
General Anesthesia
- Anesthesia response (AR) includes decreased heart rate (HR), blood pressure (BP), respiratory rate (RR), and gastrointestinal (GI) activity (nausea/vomiting).
- Emergency airway equipment must be readily available.
- Vital signs (vs) should be closely monitored.
- Safety measures include siderails and continuous monitoring until patient recovery.
Moderate Sedation
- Commonly used for minor surgical procedures (e.g., EGD, cardioversion, colonoscopy).
- AR involves decreased HR, BP, and RR; patients may be unable to protect their airway.
- Midazolam (Benzodiazepine) is administered via IV push, induces amnesia, has rapid onset, and can cause respiratory depression requiring resuscitative equipment.
- Etomidate, an IV anesthetic, has a quick onset (1 min) and rapid recovery (3-5 min), used for acute situations like rapid intubation; may cause seizure-like activity and nausea/vomiting.
- Ketamine increases HR and BP, beneficial in cardiac depression scenarios; acts quickly (30 seconds onset) with 45 min recovery, enhances effects of paralytics.
- Propofol has a rapid onset (30-60 seconds) and is used for short procedures or maintenance of sedation; must be used correctly to avoid infection, has associated risks such as localized burning.
Continuous Sedation
- Primarily used for long-term sedation in ICU settings.
- AR includes decreased RR, HR, BP, and skin breakdown due to immobility.
- Propofol is effective for quick sedation but also raises triglycerides; requires tube changes every 12 hours to reduce infection risk; can cause green urine.
- Midazolam may be used alongside low blood pressure scenarios.
- Fentanyl functions as an analgesic and sedative; assessed with the FLACC scale; has risks like respiratory depression and constipation; Narcan is available for overdose.
- Precedex, anxiolytic/hypnotic, alleviates anxiety; can either decrease or increase HR and BP depending on patient response.
Neuromuscular Blocking Agents
- Indicated for paralysis; must provide sedative prior to administration.
- AR encompasses paralysis and apnea (100% inability to breathe independently).
- Succinylcholine has rapid onset and short duration, used before intubation; prepare for potential respiratory depression.
- Vecuronium, Rocuronium, and Pancuronium are slower to act, necessitating monitoring for prolonged paralysis risks like pressure ulcers.
Analgesics
- Opioid agonists treat moderate to severe pain.
- Opioid antagonists (e.g., Naloxone) reverse respiratory and CNS depression without analgesic effects.
- ARs include respiratory depression, orthostatic hypotension, nausea/vomiting, constipation, lightheadedness, dizziness, and pupil constriction.
- Assessments involve evaluating bowel sounds, liver and kidney function, and fall risks; documentation must happen within 30 min post IV administration or 1 hour for oral dosing.
- Fentanyl is used perioperatively and in transdermal patches for chronic pain management.
- Hydromorphone effectively treats moderate to severe pain.
- Meperidine is an alternative for patients allergic to morphine, but it has side effects of potential hypotension and nausea/vomiting.
- Morphine is applicable for moderate to severe pain, both acute and chronic.
- Naloxone is critical in managing opioid overdose situations, with attention to possible withdrawal symptoms.
Cardiac Medications
- Cardiac medications may have inotropic (increase contraction), chronotropic (increase heart rate), and dromotropic (increase conduction) effects.
- Nitroglycerin is administered sublingually (1 tab every 5 min up to 3 times); dosage is titrated in 5 mg increments for effective pain management; adverse reactions include hypotension, headaches, dizziness, and weakness; caution when used with PDE5 inhibitors like Viagra.
- Digoxin, a cardiac glycoside, is used to control heart rate in atrial fibrillation (A-Fib) and heart failure scenarios.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.