Podcast
Questions and Answers
What is the primary goal of maintaining surgical anesthesia during a procedure?
What is the primary goal of maintaining surgical anesthesia during a procedure?
- To minimize anesthetic depth throughout the surgery
- To ensure rapid recovery without complications
- To maintain physiologic homeostasis and unconsciousness (correct)
- To provide amnesia and analgesia only
In Stage II of general anesthesia, which of the following signs would most likely be observed?
In Stage II of general anesthesia, which of the following signs would most likely be observed?
- Loss of conscious control with involuntary movements (correct)
- Pupillary reaction to light is reliable
- Regular and deep respirations
- Complete absence of responses to pain stimuli
Which of the following statements about Stage III of surgical anesthesia is true?
Which of the following statements about Stage III of surgical anesthesia is true?
- It consists of only one plane of anesthesia suitable for surgery.
- It is marked by the patient's ability to respond to verbal commands.
- All muscle tone is retained throughout this stage.
- There is loss of lid reflex and regular respirations. (correct)
What is a critical step in emergence preparation to avoid complications for a patient recovering from anesthesia?
What is a critical step in emergence preparation to avoid complications for a patient recovering from anesthesia?
During which stage of general anesthesia is the risk of aspiration highest, and extubation should only be done when the patient is fully awake?
During which stage of general anesthesia is the risk of aspiration highest, and extubation should only be done when the patient is fully awake?
What is the primary indication for conducting deep extubation?
What is the primary indication for conducting deep extubation?
Which of the following is a criterion for awake extubation?
Which of the following is a criterion for awake extubation?
In which situation would deep extubation be considered contraindicated?
In which situation would deep extubation be considered contraindicated?
What parameter indicates that adequate spontaneous ventilation is achieved for extubation?
What parameter indicates that adequate spontaneous ventilation is achieved for extubation?
Which of the following reflects a common misconception regarding deep extubation?
Which of the following reflects a common misconception regarding deep extubation?
What is the minimum tidal volume suggested for adequate spontaneous ventilation in patients?
What is the minimum tidal volume suggested for adequate spontaneous ventilation in patients?
Which of the following describes Monitored Anesthesia Care?
Which of the following describes Monitored Anesthesia Care?
When is a general anesthetic indicated based on patient response?
When is a general anesthetic indicated based on patient response?
What criterion is NOT a factor during deep extubation assessment?
What criterion is NOT a factor during deep extubation assessment?
What is crucial to ensure before extubation occurs?
What is crucial to ensure before extubation occurs?
Which statement best describes an important aspect of maintaining anesthetic depth?
Which statement best describes an important aspect of maintaining anesthetic depth?
What happens if a patient regains consciousness during a monitored anesthesia care procedure?
What happens if a patient regains consciousness during a monitored anesthesia care procedure?
What should be confirmed in a patient before performing a deep extubation?
What should be confirmed in a patient before performing a deep extubation?
What does adequate spontaneous ventilation involve?
What does adequate spontaneous ventilation involve?
Which is the primary goal of the anesthesiology team during deep extubation?
Which is the primary goal of the anesthesiology team during deep extubation?
Flashcards are hidden until you start studying
Study Notes
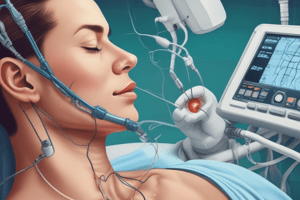
Maintenance of Surgical Anesthesia
- Involves management of physiological functions and maintenance of anesthesia from induction to emergence.
- Goals include maintaining physiologic homeostasis and ensuring unconsciousness, amnesia, analgesia, immobility, muscle relaxation, and control of sympathetic nervous system.
- Combination of inhaled and IV drugs is utilized depending on the procedure.
Fluid Management
- Maintain euvolemia for normotensive patients.
- Traditional approach vs. goal-directed fluid replacement strategy.
- Monitor urine output and replace fluids as needed during NPO or bowel prep.
Maintenance Monitoring
- Continuous vigilance is required to monitor:
- Oxygenation and vital signs
- Anesthetic depth and muscle relaxation
- Patient positioning to prevent nerve injury
Stages of General Anesthesia
- Stage I (Analgesia): Starts with induction agents, ends with loss of consciousness.
- Stage II (Delirium): Characterized by excitation, involuntary movements, and unstable vital signs.
- Stage III (Surgical Anesthesia): Deep sleep with four distinct planes; most surgeries occur here.
- Stage IV (Overdose): Total respiratory paralysis; must be reversed to prevent circulatory collapse.
Emergence from Anesthesia
- Transition from anesthesia to consciousness involves recovery of airway reflexes.
- Tailor emergence plans based on patient's comorbidities and surgical needs.
- Administer reversal agents and assess level of paralysis, ensuring adequate recovery before extubation.
Awake vs. Deep Extubation
- Awake extubation occurs when the patient responds to commands and breathes spontaneously.
- Deep extubation is used to prevent 'bucking' during emergence in suitable candidates.
Monitored Anesthesia Care (MAC)
- A service facilitating varied levels of sedation and maintaining patient comfort during procedures.
- The anesthesia provider must be ready to transition to general anesthesia if needed.
- Key for ensuring vital functions are supported throughout the procedure.
Sedation Levels and Characteristics
- Minimal Sedation (Anxiolysis): Patients respond to verbal commands; airway reflexes intact.
- Moderate Sedation/Analgesia (Conscious Sedation): Patients can respond to commands; maintain a patent airway.
- Deep Sedation/Analgesia: Patients not easily aroused; may require airway assistance; maintains cardiovascular stability.
Risks and Considerations
- Oversedation and respiratory collapse are frequent issues leading to claims in MAC.
- Certain patients (children, confused, uncooperative) may not be good candidates for MAC.
- Continuous monitoring and accessible airway equipment are crucial.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.