Podcast
Questions and Answers
What is the primary objective of advanced airway management?
What is the primary objective of advanced airway management?
- To administer medications directly into the lungs.
- To perform advanced airway management.
- To control the rate and depth of the patient's breathing.
- To clear a blocked airway and ensure effective ventilation. (correct)
What is the normal range for respiration rate in breaths per minute?
What is the normal range for respiration rate in breaths per minute?
- 25-35
- 30-40
- 8-10
- 12-20 (correct)
A respiratory rate of greater than 30 breaths per minute is considered:
A respiratory rate of greater than 30 breaths per minute is considered:
- Fast (correct)
- Slow
- Normal
- Intermediate
Which breathing pattern is characterized by a progressive increase in rate and volume, then gradually subsiding, and is often associated with head trauma?
Which breathing pattern is characterized by a progressive increase in rate and volume, then gradually subsiding, and is often associated with head trauma?
Intermittent gasping respirations in an apneic patient are best described as:
Intermittent gasping respirations in an apneic patient are best described as:
Which breathing pattern is often associated with diabetic coma?
Which breathing pattern is often associated with diabetic coma?
What is the most sensitive indicator of hypoxia?
What is the most sensitive indicator of hypoxia?
Tachycardia as a symptom of a hypoxic emergency is best described as:
Tachycardia as a symptom of a hypoxic emergency is best described as:
Which of the following is considered a late and unreliable sign of a hypoxic emergency?
Which of the following is considered a late and unreliable sign of a hypoxic emergency?
Which of the following is a breath sound associated with upper airway obstruction?
Which of the following is a breath sound associated with upper airway obstruction?
Gurgling sounds in the upper airway typically indicate:
Gurgling sounds in the upper airway typically indicate:
Snoring breath sounds indicate which of the following conditions?
Snoring breath sounds indicate which of the following conditions?
Rattling inspiratory breath sounds, which are caused by fluid in the alveoli are best described as:
Rattling inspiratory breath sounds, which are caused by fluid in the alveoli are best described as:
Continuous rattling sounds like snoring but with a quieter musical character heard in the lower airways are called:
Continuous rattling sounds like snoring but with a quieter musical character heard in the lower airways are called:
What condition is indicated by expiratory sounds caused by air being forced through narrowed bronchioles?
What condition is indicated by expiratory sounds caused by air being forced through narrowed bronchioles?
In trauma patients, which manual maneuver is recommended to open the airway?
In trauma patients, which manual maneuver is recommended to open the airway?
What is the primary reason to use manual maneuvers when managing a patient's airway?
What is the primary reason to use manual maneuvers when managing a patient's airway?
When should supplemental oxygen be considered for a patient?
When should supplemental oxygen be considered for a patient?
Which of the following ventilation techniques are considered assisted ventilation?
Which of the following ventilation techniques are considered assisted ventilation?
What are the two listed methods for providing assisted ventilation?
What are the two listed methods for providing assisted ventilation?
Why is a needle cricothyroidotomy considered a temporary procedure?
Why is a needle cricothyroidotomy considered a temporary procedure?
What are the indications for a needle cricothyroidotomy?
What are the indications for a needle cricothyroidotomy?
What is the first landmark you need to identify when performing a needle cricothyroidotomy?
What is the first landmark you need to identify when performing a needle cricothyroidotomy?
What is the most crucial step to complete before beginning the needle cricothyroidotomy procedure?
What is the most crucial step to complete before beginning the needle cricothyroidotomy procedure?
What size sheathed needle catheter is recommended for performing a needle cricothyroidotomy?
What size sheathed needle catheter is recommended for performing a needle cricothyroidotomy?
What is the correct insertion angle when introducing the catheter into the subcutaneous tissue during a needle cricothyroidotomy?
What is the correct insertion angle when introducing the catheter into the subcutaneous tissue during a needle cricothyroidotomy?
During a needle cricothyroidotomy, at what angle should you advance the catheter into the larynx after air return?
During a needle cricothyroidotomy, at what angle should you advance the catheter into the larynx after air return?
Why is it critical to hold the catheter securely following placement and during ventilation when performing a needle cricothyroidotomy?
Why is it critical to hold the catheter securely following placement and during ventilation when performing a needle cricothyroidotomy?
Following a needle cricothyroidotomy, what airway interventions are acceptable?
Following a needle cricothyroidotomy, what airway interventions are acceptable?
What is the typical purpose of using a ventilator?
What is the typical purpose of using a ventilator?
What does PEEP stand for in the context of ventilation?
What does PEEP stand for in the context of ventilation?
What does the measurement of tidal volume (TV) represent?
What does the measurement of tidal volume (TV) represent?
In the context of ventilation, "peak pressure" refers to:
In the context of ventilation, "peak pressure" refers to:
What does FiO2 represent in respiratory care?
What does FiO2 represent in respiratory care?
What does the acronym EMMA stand for in the context of respiratory monitoring?
What does the acronym EMMA stand for in the context of respiratory monitoring?
What is the primary function of a Heat and Moisture Exchanger (HME) in ventilator use?
What is the primary function of a Heat and Moisture Exchanger (HME) in ventilator use?
On the SAVE II ventilator, what does the confirmation button primarily do?
On the SAVE II ventilator, what does the confirmation button primarily do?
What is the purpose of the 'Manual Trigger' button on the SAVE II ventilator?
What is the purpose of the 'Manual Trigger' button on the SAVE II ventilator?
Where is the green side of the large bore tubing attached when adding supplemental oxygen to the SAVE II?
Where is the green side of the large bore tubing attached when adding supplemental oxygen to the SAVE II?
During ventilation with the SAVE II, what adjustments should be considered if end-tidal CO2 levels are too low?
During ventilation with the SAVE II, what adjustments should be considered if end-tidal CO2 levels are too low?
In a patient with a foreign body obstruction where ventilation is impossible, and a needle cricothyroidotomy is performed, where, anatomically is the needle inserted?
In a patient with a foreign body obstruction where ventilation is impossible, and a needle cricothyroidotomy is performed, where, anatomically is the needle inserted?
An intubated patient is being mechanically ventilated. Despite appropriate ventilator settings, their end-tidal CO2 is trending upwards. What might this indicate?
An intubated patient is being mechanically ventilated. Despite appropriate ventilator settings, their end-tidal CO2 is trending upwards. What might this indicate?
When assessing a patient's breathing quality, what qualifies as an 'intermediate' respiration rate?
When assessing a patient's breathing quality, what qualifies as an 'intermediate' respiration rate?
What characteristic defines a normal breathing rhythm?
What characteristic defines a normal breathing rhythm?
What underlying condition might Kussmaul's respirations indicate?
What underlying condition might Kussmaul's respirations indicate?
Besides level of consciousness, which of the following is the most sensitive early indicator of a hypoxic emergency?
Besides level of consciousness, which of the following is the most sensitive early indicator of a hypoxic emergency?
What is the body's initial reflex to hypoxia to maintain oxygen levels at the cellular level?
What is the body's initial reflex to hypoxia to maintain oxygen levels at the cellular level?
What does cyanosis indicate in the context of a hypoxic emergency?
What does cyanosis indicate in the context of a hypoxic emergency?
When assessing breath sounds, what is an expected finding in all lung fields?
When assessing breath sounds, what is an expected finding in all lung fields?
What does the presence of stridor indicate?
What does the presence of stridor indicate?
Rales indicates what condition is occurring in the lower airways?
Rales indicates what condition is occurring in the lower airways?
What can the presence of wheezing indicates
What can the presence of wheezing indicates
During a primary assessment, what element of a patient's history requires cervical spine protection?
During a primary assessment, what element of a patient's history requires cervical spine protection?
What manual maneuver is most appropriate for opening the airway of a patient with suspected cervical spine injury?
What manual maneuver is most appropriate for opening the airway of a patient with suspected cervical spine injury?
When is supplemental oxygen indicated?
When is supplemental oxygen indicated?
Assisted ventilations are indicated when?
Assisted ventilations are indicated when?
What are acceptable methods for providing assisted ventilation?
What are acceptable methods for providing assisted ventilation?
During a needle cricothyroidotomy, what is the catheter inserted into?
During a needle cricothyroidotomy, what is the catheter inserted into?
Why is a needle cricothyroidotomy considered a temporary solution for airway management?
Why is a needle cricothyroidotomy considered a temporary solution for airway management?
What is a primary indication for performing a needle cricothyroidotomy?
What is a primary indication for performing a needle cricothyroidotomy?
When preparing to perform a needle cricothyroidotomy, which of the following is the first anatomical landmark that must be identified?
When preparing to perform a needle cricothyroidotomy, which of the following is the first anatomical landmark that must be identified?
Before beginning a needle cricothyroidotomy, what crucial step must be completed?
Before beginning a needle cricothyroidotomy, what crucial step must be completed?
What is the suggested gauge size for the sheathed needle catheter used in a needle cricothyroidotomy?
What is the suggested gauge size for the sheathed needle catheter used in a needle cricothyroidotomy?
During a needle cricothyroidotomy, at what angle to the skin should the catheter be introduced initially?
During a needle cricothyroidotomy, at what angle to the skin should the catheter be introduced initially?
When advancing the catheter into the larynx during a needle cricothyroidotomy, at what angle should the catheter be positioned after confirming air return?
When advancing the catheter into the larynx during a needle cricothyroidotomy, at what angle should the catheter be positioned after confirming air return?
Why is it important to securely hold the catheter following placement and during ventilation in a needle cricothyroidotomy?
Why is it important to securely hold the catheter following placement and during ventilation in a needle cricothyroidotomy?
Following successful completion of a needle cricothyroidotomy, what is the next step in airway management?
Following successful completion of a needle cricothyroidotomy, what is the next step in airway management?
How does Positive End-Expiratory Pressure (PEEP) assist in ventilation?
How does Positive End-Expiratory Pressure (PEEP) assist in ventilation?
What does 'peak pressure' refer to when discussing ventilation?
What does 'peak pressure' refer to when discussing ventilation?
What is the role of the EMMA device during respiratory support?
What is the role of the EMMA device during respiratory support?
How does a Heat and Moisture Exchanger (HME) function in the context of ventilator use?
How does a Heat and Moisture Exchanger (HME) function in the context of ventilator use?
Following the set-up steps correctly, what is the third thing you should do to start-up the SAVE II ventilator?
Following the set-up steps correctly, what is the third thing you should do to start-up the SAVE II ventilator?
On the SAVE II ventilator, after set-up, what are the next steps?
On the SAVE II ventilator, after set-up, what are the next steps?
Flashcards
Patent airway
Patent airway
Ensuring the patient has an unobstructed and open airway.
Cheyne-Stokes Breathing
Cheyne-Stokes Breathing
Disturbance in respiratory center; breathing rate/volume increases then subsides. Associated with head trauma.
Agonal Respirations
Agonal Respirations
Intermittent gasps as a reflex on an apneic patient.
Kussmaul Breathing
Kussmaul Breathing
Signup and view all the flashcards
Level of consciousness
Level of consciousness
Signup and view all the flashcards
Tachycardia (in hypoxia)
Tachycardia (in hypoxia)
Signup and view all the flashcards
Cardiac dysrhythmias (in hypoxia)
Cardiac dysrhythmias (in hypoxia)
Signup and view all the flashcards
Cyanosis
Cyanosis
Signup and view all the flashcards
Snoring
Snoring
Signup and view all the flashcards
Gurgling
Gurgling
Signup and view all the flashcards
Stridor
Stridor
Signup and view all the flashcards
Rales
Rales
Signup and view all the flashcards
Rhonchi
Rhonchi
Signup and view all the flashcards
Wheezing
Wheezing
Signup and view all the flashcards
Trauma
Trauma
Signup and view all the flashcards
Manual maneuvers
Manual maneuvers
Signup and view all the flashcards
Maintaining airway/head position
Maintaining airway/head position
Signup and view all the flashcards
Manual First
Manual First
Signup and view all the flashcards
Oxygenation
Oxygenation
Signup and view all the flashcards
Assisted ventilations
Assisted ventilations
Signup and view all the flashcards
Needle Cricothyroidotomy
Needle Cricothyroidotomy
Signup and view all the flashcards
Needle Cricothyroidotomy: Indications
Needle Cricothyroidotomy: Indications
Signup and view all the flashcards
Landmarks for Cricothyroidotomy
Landmarks for Cricothyroidotomy
Signup and view all the flashcards
Structures to avoid
Structures to avoid
Signup and view all the flashcards
Positive End-Expiratory Pressure (PEEP)
Positive End-Expiratory Pressure (PEEP)
Signup and view all the flashcards
Tidal Volume (TV)
Tidal Volume (TV)
Signup and view all the flashcards
Peak Pressure
Peak Pressure
Signup and view all the flashcards
Fraction of Inspired Oxygen (Fi02)
Fraction of Inspired Oxygen (Fi02)
Signup and view all the flashcards
Emergency Mainstream Analyzer (EMMA)
Emergency Mainstream Analyzer (EMMA)
Signup and view all the flashcards
Heat and Moisture Exchanger (HME)
Heat and Moisture Exchanger (HME)
Signup and view all the flashcards
Study Notes
- Unit 5 is about Airway Management
- Objective: Perform advanced airway management
Overview of Airway Management Topics
- Advanced Airway Management
- Needle Cricothyroidotomy
- SAVe II Ventilator
Basic Airway Management
- Assessment includes ensuring a patent airway, looking for spontaneous chest rise and fall, listening for air movement, and feeling for air movement.
Assess Quality of Breathing
- Assess Rate (per minute)
- Slow is less than 12
- Normal is 12-20
- Intermediate is 20-30
- Fast is greater than 30
- Assess Rhythm; it should be regular
- Cheyne-Stokes rhythm is associated with disturbance in respiratory center, such as head trauma
- Cheyne-Stokes rhythm is characterized by progressive increase in rate and volume, then gradually subsiding
- Agonal respirations are intermittent gasps as a reflex on an apneic patient
- Assess Depth
- Deep-Kussmaul is a very deep gasping pattern often associated with diabetic coma
- Shallow can be caused by hyperventilation and guarded respirations due to pain, resulting in incomplete breaths
- Signs of Hypoxic Emergencies
- Level of consciousness is one of the most sensitive indicators of hypoxia
- Anxiety/dyspnea
- Tachycardia is the body's reflex towards maintaining adequate oxygen levels at the cellular levels by speeding up the flow of the remaining oxygenated blood
- Cardiac dysrhythmias may be caused by myocardial hypoxia
- Cyanosis is a late sign and not considered dependable for early warning
- Check Breath Sounds
- They should be present and equal in all fields
- Abnormal sounds are separated into upper and lower airway
Abnormal Breath Sounds
- Upper Airway
- Snoring: partial obstruction of upper airway by the tongue
- Gurgling: accumulation of blood, vomitus or secretions in the upper airway
- Stridor: harsh, high-pitched, sound heard on inhalation associated with laryngeal edema or constriction
- Lower Airway
- Rales: Rattling inspiratory breath sound due to fluid in alveoli, which may be a result of CHF, AMI, PE, burns to lower airway, drowning, runaway IV's, or pneumonia
- Rhonchi: Continuous inspiratory or expiratory rattling sound similar to snoring but with a quieter musical character
- Wheezing: Expiratory sound caused by air being forced through narrowing bronchioles; may be heard with asthma, anaphylaxis or possible PE
- Other abnormal sounds are rarely found during emergency care
Considerations for Patient History
- Trauma: always protect C-Spine; review history for indications of trauma to the head, neck, chest, and upper extremities
- Foreign Body aspiration or ingestion such as food, vomit, or blood clots
- Environmental exposure: Allergens, gases and chemical vapors, and burns
Secure the Airway
- Manual Maneuvers
- Head tilt/chin lift (non-trauma)
- Jaw thrust (trauma); intended for patients with possibility of cervical spine injuries
- Basic Mechanical Airways: Maintaining the airway/head position is always important when using basic mechanical airways
- Establish an airway using manual maneuvers prior to mechanical attempts
- Delays in securing the airway can be life threatening
- Oropharyngeal and nasal pharyngeal airways (OPA/NPA)
- Oxygenation
- Supplemental Oxygen should be considered for any patient whose history or condition may lead to respiratory or circulatory collapse (shock)
- Options for providing oxygen include a nasal cannula, simple face mask, and non-rebreather mask with reservoir
- Ventilation
- Assisted ventilations are not just for the apneic patient
- Patients with respiratory rates outside the normal range or with dyspnea will need assisted ventilations to maintain adequate
- Methods of ventilation include mouth to mask and bag-valve mask (BVM)
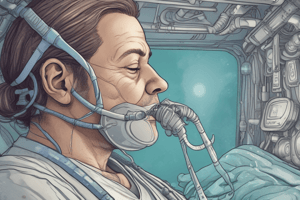
Needle Cricothyroidotomy
- Access to the airway is gained through a needle insertion into the cricoid membrane
- The procedure is a temporary means to allow immediate ventilation of the patient with an obstructed airway.
- It does not provide adequate ventilation and is only a temporary solution until a definitive airway can be established
- Followed by surgical insertion of an endotracheal tube
Needle Cricothyroidotomy Procedure
- Indications include upper airway obstruction prohibiting ventilation or intubation and cervical spine injuries considered unacceptable for intubation
- Identify Landmarks includes the Cricoid cartilage, Thyroid cartilage, and Cricothyroid membrane
- Identify vital structures such as the carotid arteries, esophagus, and trachea which may be injured by incorrect technique
- Place patient supine, with the neck straight and not angulated
- Time permitting, apply provident-iodine solution to the skin
- Ventilate with BVM connected to O2 while gathering supplies
Gather Supplies for Needle Cricothyroidotomy
- PPE
- 16G or larger sheathed needle catheter
- 3 ml syringe
- Adaptor from the end of a 7-mm endotracheal tube
- O2 source at 15 L/min connected by tubing with a Y connector or fashioned with side hole
- A BVM may be substituted but not optimal
Perform Needle Cricothyroidotomy
- Stand to side of patient at level of neck
- Locate cricothyroid membrane
- Attach 3ml syringe to catheter (16 gauge or larger)
- Introduce the catheter into the subcutaneous tissue at a 90-degree angle to the skin
- Aspirate gently while advancing catheter over the needle
- When air returns (indicating entry into the airway), change angle to 45 degrees and advance catheter into larynx
- Withdraw needle and syringe
- Disconnect 3ml syringe from
- Withdraw plunger from 3mm syringe and attach plunger-less 3ml syringe barrel to the catheter in the neck
- Attach the adapter from end of 7mm ETT into the empty syringe barrel and inflate balloon
- Attach the O2 source to the adapter and start ventilation w/ a 100% O2 source
- The operator must hold the catheter securely, as it can become displaced with minimal movement
- Stabilization is maintained by the operator until choice of airway is established, using either tracheostomy or orotracheal or nasotracheal intubation (if possible)
- Dressings are not necessary
SAVe II Ventilator
- Purpose: If a patient has diminished function of their lungs or the inability to breath on their own, then a ventilator can assist with breathing or completely breath for them.
- Delivers oxygen and pressure to the patient, and can be configured
- It is important to have knowledge of basic terminology and mechanics to understand how the ventilator works
Terminology for SAVe II Ventilator
- Positive End-Expiratory Pressure (PEEP): Positive pressure that will remain in the airway at the end if the respiratory cycle that is greater than the atmospheric pressure or the pressure outside the body
- Tidal Volume (TV): A measurement of the amount of air an individual inhales and exhales during a normal breath
- Peak Pressure: Pressure generated by the ventilator to overcome airway resistance and alveolar resistance to attain peak inspiratory flow and to deliver desired tidal volume
- Fraction of Inspired Oxygen (Fi02): The percentage or concentration of oxygen that is inhaled
- Emergency Mainstream Analyzer (EMMA): Emergency Capnometer for proof-of-intubation and short-term C02 monitoring in emergency transports/situations
- Measures end-tidal CO2 and respiratory rate
- Heat and Moisture Exchanger (HME): Humidifies and filters air to help reduce mucus production and coughing
SAVe II Ventilator Overview
- Components indicated on the device include the power button, alarm silence, height selection, single manual breath, respiratory rate, tidal volume, PEEP, peak pressure limit, and confirmation button.
SAVe II Ventilator Start-Up
- Press power
- Select patient height
- Press confirm
- Add PEEP/Start Ventilator
- Press confirm
- Increase PEEP to 5
- If different Tidal Volume is desired, refer to the chart to determine the correct setting
Supplemental Oxygen for SAVe II Ventilator
- Remove black cap (do not discard cap or white filter)
- Attach green side of large bore tubing to vent
- Fully extend large bore tubing
- Attach small bore tubing to O2 and turn flow to 6 LPM
Monitoring the Patient on SAVe II Ventilator
- Maintain end tidal CO2 between 35-45 mmHg
- Increase respiratory rate (RR) or tidal volume (TV) to lower end tidal CO2
- Decrease RR or TV to raise end tidal CO2
- Maintain SpO2 above 94%
- Increase FiO2 or PEEP to raise
Recommended Adjunct Placement
- Suction
- EMMA
- HME
- Metered-dose in
- Nebulizer (NEB)
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.