Podcast
Questions and Answers
What is the definition of acute respiratory failure (ARF)?
What is the definition of acute respiratory failure (ARF)?
A condition in which the respiratory system fails in one or both of its gas-exchange functions, namely oxygenation and elimination of Carbon Dioxide (CO2)
What are the conventional criteria for defining acute respiratory failure?
What are the conventional criteria for defining acute respiratory failure?
PaO2 < 60 mmHg and/or PaCO2 > 45 mmHg & pH < 7.35, or both
What is the normal range for PaO2 in arterial blood?
What is the normal range for PaO2 in arterial blood?
80-100 mmHg
What is the general treatment for acute respiratory failure?
What is the general treatment for acute respiratory failure?
What are the two components of the respiratory system that can fail, leading to respiratory failure?
What are the two components of the respiratory system that can fail, leading to respiratory failure?
What is the difference between Type I and Type II respiratory failure?
What is the difference between Type I and Type II respiratory failure?
What are the two main categories of causes of acute respiratory failure?
What are the two main categories of causes of acute respiratory failure?
What are some common clinical features of acute respiratory failure?
What are some common clinical features of acute respiratory failure?
What is the most common cause of hypoxaemia in respiratory failure?
What is the most common cause of hypoxaemia in respiratory failure?
What are the determinants of gas exchange in the lungs?
What are the determinants of gas exchange in the lungs?
What is the main difference between a shunt and dead space in V/Q mismatch?
What is the main difference between a shunt and dead space in V/Q mismatch?
What is the main difference between Type 1 and Type 2 respiratory failure?
What is the main difference between Type 1 and Type 2 respiratory failure?
What is the primary goal of managing respiratory failure?
What is the primary goal of managing respiratory failure?
What is the priority in managing respiratory failure?
What is the priority in managing respiratory failure?
What is the main difference between stagnant hypoxia and anemic hypoxia?
What is the main difference between stagnant hypoxia and anemic hypoxia?
What are the early and late respiratory features of hypoxia?
What are the early and late respiratory features of hypoxia?
What are the effects of hypercarbia on the oxy-haemoglobin dissociation curve?
What are the effects of hypercarbia on the oxy-haemoglobin dissociation curve?
What are the clinical manifestations of hypercarbia at different levels of PaCO2?
What are the clinical manifestations of hypercarbia at different levels of PaCO2?
What is the main cause of Type II respiratory failure?
What is the main cause of Type II respiratory failure?
What is the effect of hypoxia on the cardiovascular system?
What is the effect of hypoxia on the cardiovascular system?
What is the effect of hypoxia on the neurological system?
What is the effect of hypoxia on the neurological system?
What is the effect of hypercarbia on the respiratory system?
What is the effect of hypercarbia on the respiratory system?
whats the Mechanisms of hypoxaemia
whats the Mechanisms of hypoxaemia
example of shunt
example of shunt
example of dead space ventilation
example of dead space ventilation
Determinates of Gas Exchange
Determinates of Gas Exchange
What are the causes of hypoxia in acute respiratory failure?
What are the causes of hypoxia in acute respiratory failure?
Who is at risk of CO2 retention
Who is at risk of CO2 retention
Management of Respiratory Failure-Failure to oxygenate
Management of Respiratory Failure-Failure to oxygenate
Management of Respiratory Failure-Failure to ventilate
Management of Respiratory Failure-Failure to ventilate
mechanisms' of hypercarbia
mechanisms' of hypercarbia
Flashcards are hidden until you start studying
Study Notes
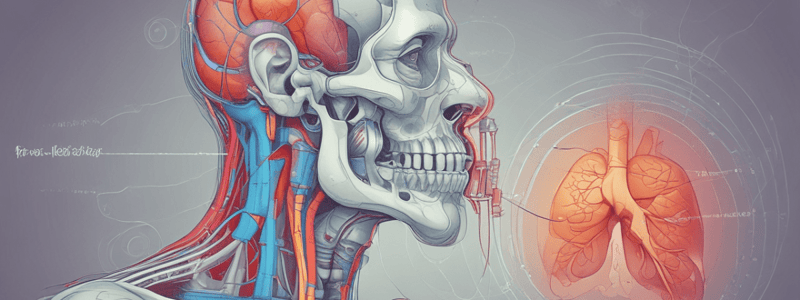
Acute Respiratory Failure (ARF)
- Defined as a condition in which the respiratory system fails in one or both of its gas-exchange functions: oxygenation and elimination of carbon dioxide
- Classified into two types: Type I (Failure to Oxygenate) and Type II (Failure to Ventilate)
Type I Respiratory Failure: Failure to Oxygenate
- Characterized by hypoxaemia (PaO2 < 60 mmHg)
- Mechanisms of hypoxaemia: low fraction of inspired oxygen (FiO2), V/Q mismatch, diffusion defect
- Causes: intrapulmonary diseases (COPD, pneumonia), extrapulmonary diseases (pulmonary oedema, cardiac failure), and others
Type II Respiratory Failure: Failure to Ventilate
- Characterized by hypercapnia (PaCO2 > 45 mmHg) and usually accompanied by hypoxaemia
- Caused by hypoventilation due to various factors such as central nervous system disorders, peripheral nervous system disorders, and others
Clinical Features of Acute Respiratory Failure
- Variable and dependent on the underlying cause, degree of hypoxaemia, hypercarbia, and acidosis
- Symptoms: dyspnoea, tachypnoea, orthopnoea, inability to speak, use of accessory muscles, intercostal retractions, paradoxical abdominal movement, noisy breathing, anxiety, restlessness, confusion, lethargy, and coma
Mechanisms and Features of Hypoxaemia
- Defined as deficient oxygenation of arterial blood (PaO2 < 80 mmHg)
- Causes: stagnant hypoxia, anaemic hypoxia, histotoxic hypoxia
- Clinical features: respiratory, cardiovascular, neurological, and skin-related symptoms
Mechanisms and Features of Hypercarbia
- Defined as deficient elimination of carbon dioxide (PaCO2 > 45 mmHg)
- Causes: hypoventilation due to various factors
- Clinical features: tachypnoea, dyspnoea, headache, restlessness, agitation, confusion, coma, and death in severe cases
Management of Respiratory Failure
- General goals of therapy: maintain airway patency, optimise oxygen delivery, optimise CO and ensure adequate Hb, minimise oxygen demand, identify and treat the underlying cause, and prevent complications
- Specific therapies: oxygen therapy, NIV, IPPV, PEEP, CPAP, and others
ABG Analysis and Interpretation
- VBG and ABG normal values: pH, PvO2, PvCO2, HCO3-, BE
- Interpretation of ABG results: assessment of oxygenation, ventilation, and acid-base status
Case Study
- 25-year-old female with mild SOB and chest pain, presented to ED with negative cardiac troponin level
- ABG results: PaO2 = 70 mmHg, pH = 7.25, PaCO2 = 51 mmHg, HCO3- = 24 mEq/L
- Diagnosis and management of acute respiratory failure
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.