Podcast
Questions and Answers
Under what circumstances would the concentration of an acid and its conjugate base be most effective in buffering a solution?
Under what circumstances would the concentration of an acid and its conjugate base be most effective in buffering a solution?
- When the concentration of the conjugate base is negligible.
- When the concentrations of the acid and the conjugate base are approximately equal. (correct)
- When the solution is devoid of other ions.
- When the concentration of the acid is much greater than that of the conjugate base.
How does the body respond to an increase in the partial pressure of CO2 (pCO2) or a decrease in pH?
How does the body respond to an increase in the partial pressure of CO2 (pCO2) or a decrease in pH?
- Decreasing alveolar ventilation to retain CO2.
- Suppressing the brain respiratory control center.
- Reducing the rate of CO2 excretion proportionally.
- Increasing alveolar ventilation to eliminate CO2. (correct)
In the context of acid-base balance, what is the physiological significance of regulating the partial pressure of CO2 (pCO2) in body fluids?
In the context of acid-base balance, what is the physiological significance of regulating the partial pressure of CO2 (pCO2) in body fluids?
- To control the concentration of nonvolatile acids in the body.
- To influence the concentration of carbonic acid (H2CO3), a key component of the pH regulatory process. (correct)
- To ensure adequate oxygen delivery to tissues.
- To maintain a constant level of bicarbonate ions (HCO3-) in the blood.
How do the kidneys compensate when non-volatile acids accumulate in the body, leading to a decrease in pH?
How do the kidneys compensate when non-volatile acids accumulate in the body, leading to a decrease in pH?
What condition is indicated when arterial blood samples reveal abnormal pH, pCO2, and/or [HCO3-] values?
What condition is indicated when arterial blood samples reveal abnormal pH, pCO2, and/or [HCO3-] values?
In the context of acid-base balance, what occurs when carbonic acid is dehydrated to CO2?
In the context of acid-base balance, what occurs when carbonic acid is dehydrated to CO2?
According to the Henderson-Hasselbalch equation, what three variables are related such that if any two are known, the third can be calculated?
According to the Henderson-Hasselbalch equation, what three variables are related such that if any two are known, the third can be calculated?
In the context of acid-base buffering, what explains that the imidazole group of histidine is particularly effective at physiological pH?
In the context of acid-base buffering, what explains that the imidazole group of histidine is particularly effective at physiological pH?
In the titration of body fluids, what is added to the solution when carbonic acid is produced by increasing dissolved CO2?
In the titration of body fluids, what is added to the solution when carbonic acid is produced by increasing dissolved CO2?
Why should the compensatory rise in [HCO3-] in metabolic alkalosis NOT be termed "metabolic acidosis?"
Why should the compensatory rise in [HCO3-] in metabolic alkalosis NOT be termed "metabolic acidosis?"
What does the Davenport diagram reveal about the acid-base balance in the human body?
What does the Davenport diagram reveal about the acid-base balance in the human body?
Which statement accurately describes the direct effect of aldosterone on acid-base balance within the kidneys?
Which statement accurately describes the direct effect of aldosterone on acid-base balance within the kidneys?
What is a key difference between carbonic and non-carbonic acid in body fluid titration?
What is a key difference between carbonic and non-carbonic acid in body fluid titration?
Why is respiratory compensation for metabolic alkalosis limited by hypoxia?
Why is respiratory compensation for metabolic alkalosis limited by hypoxia?
What is the primary mechanism by which non-carbonic acids are buffered in the extracellular fluid (ECF)?
What is the primary mechanism by which non-carbonic acids are buffered in the extracellular fluid (ECF)?
In a patient presenting with chronic hypercapnia, what is the limiting factor for renal compensation?
In a patient presenting with chronic hypercapnia, what is the limiting factor for renal compensation?
How does total body potassium depletion lead to extracellular acidosis?
How does total body potassium depletion lead to extracellular acidosis?
Which statement reflects the interaction between plasma and intracellular pH?
Which statement reflects the interaction between plasma and intracellular pH?
What is the primary mechanism by which the kidneys contribute to the compensation of respiratory acidosis?
What is the primary mechanism by which the kidneys contribute to the compensation of respiratory acidosis?
Why are strong electrolytes particularly effective at influencing the electrolytic balance in solutions?
Why are strong electrolytes particularly effective at influencing the electrolytic balance in solutions?
How does increased lactic acid production result in the tendency for pH to normalize in cases of respiratory alkalosis?
How does increased lactic acid production result in the tendency for pH to normalize in cases of respiratory alkalosis?
How does the body biochemically respond to a rise in pCO2?
How does the body biochemically respond to a rise in pCO2?
What is the effect on the rate of nonvolatile (non-carbonic) acid secretion and excretion by the kidneys when the partial pressure of CO2 (pCO2) rises, or the pH decreases?
What is the effect on the rate of nonvolatile (non-carbonic) acid secretion and excretion by the kidneys when the partial pressure of CO2 (pCO2) rises, or the pH decreases?
What characterizes the relationship between the quantities pCO2, pH, and [HCO3-] even across a broad spectrum of acid-base disorders?
What characterizes the relationship between the quantities pCO2, pH, and [HCO3-] even across a broad spectrum of acid-base disorders?
How is the non-carbonic acid content regulated in the body?
How is the non-carbonic acid content regulated in the body?
What is the function of hemoglobin in buffering acids or bases added to the extracellular fluid (ECF)?
What is the function of hemoglobin in buffering acids or bases added to the extracellular fluid (ECF)?
In a scenario where a patient has a blood pH of 7.37, a pCO2 of 60 mmHg, and an HCO3- concentration of 34 mEq/L, what compensatory mechanism is most likely occurring over time?
In a scenario where a patient has a blood pH of 7.37, a pCO2 of 60 mmHg, and an HCO3- concentration of 34 mEq/L, what compensatory mechanism is most likely occurring over time?
A patient presents with a known case of COPD and is found to have impaired gas exchange in the lungs. How does this impact acid-base balance?
A patient presents with a known case of COPD and is found to have impaired gas exchange in the lungs. How does this impact acid-base balance?
Which condition is most likely to result in the addition of β-hydroxybutyrate and acetoacetate, leading to a surplus of non-carbonic acid in the body?
Which condition is most likely to result in the addition of β-hydroxybutyrate and acetoacetate, leading to a surplus of non-carbonic acid in the body?
How should you respond to a patient who is hyperventilating?
How should you respond to a patient who is hyperventilating?
Flashcards
Acidemia
Acidemia
Condition where pH is less than 7.40 at sea level.
Alkalemia
Alkalemia
Condition where pH is greater than 7.40 at sea level.
Respiratory Imbalance
Respiratory Imbalance
Changes in carbonic acid due to ventilation changes.
Metabolic Imbalance
Metabolic Imbalance
Signup and view all the flashcards
Volatile Acid (pCO2)
Volatile Acid (pCO2)
Signup and view all the flashcards
Diabetic Ketoacidosis
Diabetic Ketoacidosis
Signup and view all the flashcards
Buffering
Buffering
Signup and view all the flashcards
Strong Electrolyte
Strong Electrolyte
Signup and view all the flashcards
Weak Electrolyte
Weak Electrolyte
Signup and view all the flashcards
Partial Pressure of CO2 (pCO2)
Partial Pressure of CO2 (pCO2)
Signup and view all the flashcards
Compensation
Compensation
Signup and view all the flashcards
Simple Acid-Base Disorder
Simple Acid-Base Disorder
Signup and view all the flashcards
Hypercapnia
Hypercapnia
Signup and view all the flashcards
Carbonic Acid Regulation
Carbonic Acid Regulation
Signup and view all the flashcards
Non-Volatile Acid Regulation
Non-Volatile Acid Regulation
Signup and view all the flashcards
Kidney Acid Secretion Factors
Kidney Acid Secretion Factors
Signup and view all the flashcards
COPD acid base unbalance
COPD acid base unbalance
Signup and view all the flashcards
Buffer
Buffer
Signup and view all the flashcards
Strong Electrolyte
Strong Electrolyte
Signup and view all the flashcards
Acid
Acid
Signup and view all the flashcards
Base
Base
Signup and view all the flashcards
Dissociation Constant K’a
Dissociation Constant K’a
Signup and view all the flashcards
Titration Curve
Titration Curve
Signup and view all the flashcards
Acid-Base Map
Acid-Base Map
Signup and view all the flashcards
Large Amount of Buffers
Large Amount of Buffers
Signup and view all the flashcards
Below 7.40
Below 7.40
Signup and view all the flashcards
Above 7.40
Above 7.40
Signup and view all the flashcards
Metabolic Alkalosis
Metabolic Alkalosis
Signup and view all the flashcards
Metabolic Acidosis
Metabolic Acidosis
Signup and view all the flashcards
Respiratory Acidosis
Respiratory Acidosis
Signup and view all the flashcards
Respiratory Alkalosis
Respiratory Alkalosis
Signup and view all the flashcards
Lungs excrete Carbonic acid
Lungs excrete Carbonic acid
Signup and view all the flashcards
kidneys excrete non-carbonic
kidneys excrete non-carbonic
Signup and view all the flashcards
Study Notes
- 2025 is the year the learning objectives are current
General Terms
- It is important to define the acid-base state of an organism and regulate pH.
- Distinguish between volatile and nonvolatile acids and bases.
- Diet composition determines which acids and bases are generated.
- Define and apply partial pressure, equilibrium, buffering, and buffer value.
- Distinguish buffering from compensation.
Types of Buffers
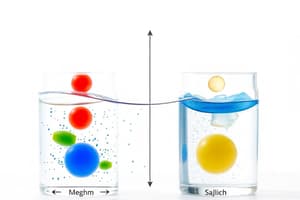
- Identify the body fluid compartments in acid-base equilibrium and how they relate.
- Hemoglobin plays a role in buffering systemic pH.
- Understand the HCO3¯/CO2 system's operation and its pivotal role in acid-base balance.
- Learn the modification of the Henderson-Hasselbalch equation relating to body pH.
- Be aware of the role of other acid-base buffers in regulating systemic pH.
Davenport Diagram
- Become familiar with applying the acid-base map to conditions.
- Show how the body titrates acids and bases at a fixed pCO2 along the isobar.
- Distinguish how body fluids are titrated with carbonic acid vs. non-carbonic acid buffers.
- Identify and quantitate base deficit and base excess.
Acid Base and its Regulation
- The Davenport diagram is a four-dimensional acid-base map.
- The X-axis is pH.
- The Y-axis is HCO3.
- pCO2 is on the isobars (curved lines).
- The hemoglobin titration curve is the slanted line.
- The body has separate but interacting fluid compartments: bone, plasma, interstitial fluid, intracellular fluid, and RBCs.
- The final acid-base state is a composite of these compartments, which may change over time.
- The acid-base state of the body is usually taken to mean the state of arterial blood or extracellular fluid (ECF).
- The pH of ECF reflects the pH of other compartments, with the simplification that ECF or arterial blood pH reflects body pH.
- pH is important because the functional activities of proteins (enzymes, transport molecules, etc.) depend on it.
Acid Production
- The body produces acid through metabolism.
- CO2 metabolic production is approximately 13,000 mmol/day.
- CO2 is removed by exhaling 300 L CO2/day and is a Class 1 volatile acid.
- Oxidation of P and S in proteins and nucleotides forms H3PO4 and H2SO4 (~70-100 mmol/day).
- These are excreted by the kidney and are Class 2 nonvolatile acids.
- The body is constantly producing acid, with more volatile acid produced than nonvolatile acid.
- Class 1 acids are volatile (carbonic acid), and Class 2 acids are non-volatile (all other acids).
- Excess acid is removed by excretion.
- Carbonic acid becomes volatile CO2 and is excreted by the lungs.
- Non-carbonic acids are excreted by the kidneys.
The CO2/HCO3 System
- pCO2 is the partial pressure of CO2, and H2CO3 is an acid.
- The body is an open system.
- Volatile acid, CO2, is controlled by intake/output by the lungs.
- Nonvolatile acid excretion is controlled by the kidneys.
- pCO2 is regulated in body fluids because it measures dissolved CO2 concentration.
- CO2 in its hydrated form, H2CO3, is an acid, with its concentration regulated as part of the pH regulatory process.
H2CO3 Regulation
-
CO2 + H2O ↔ H2CO3 ↔ H+ + HCO3-
-
The rate of CO2 excretion is proportional to alveolar ventilation.
-
Increased pCO2 leads to increased respiratory center activity, while decreased pH has the same effect.
-
Increased alveolar ventilation leads to decreased alveolar pCO2.
-
Alveolar pCO2 is in rapid equilibrium with arterial pCO2, also decreasing pH will increase toward normal.
-
The body regulates carbonic and non-carbonic acid by controlling CO2 and nonvolatile acid intake/output.
-
Increased pCO2 or decreased pH increases alveolar ventilation.
-
Increased alveolar ventilation decreases alveolar pCO2.
-
An increase in alveolar ventilation decreases alveolar pCO2, and decreases arterial pCO2 which inceases pH toward normal
-
A decrease in alveolar ventilation increases pCO2
-
Increased acid ingestion or metabolism increases H+ production.
-
Increased acid secretion leads to increased acid excretion into urine.
-
Non-volatile acid regulation is that increased H⁺ or decreased pH increases acid excretion by kidneys
-
Non-volatile acid content is determined by the rate of acid intake, production by metabolism, and excretion of H+ by kidneys.
-
An increase in volatile acid increases acid excretion by kidneys.
-
The rate of acid secretion by the kidney is controlled by pCO2 and pH.
-
Increased pCO2 or decreased pH increases non-volatile acid secretion/excretion by the kidneys.
Acid-Base Unbalance
- COPD (chronic obstructive pulmonary disease) is an impaired gas exchange in lungs; this leads to carbonic acid accumulation.
- Diabetic ketoacidosis occurs with the addition of β-hydroxybutyrate and acetoacetate leads to surplus of non-carbonic acid in the body.
- COPD causes a build-up of CO2 and carbonic acid.
- Uncontrolled diabetes mellitus with ketoacidosis causes addition of non-carbonic acids to the body.
Buffering
- Buffering is the property of a substance to reduce pH change from adding a strong acid or base.
- A weak acid or base buffers against changes in pH where acid and conjugate base concentrations are comparable (H+ + B- ↔ HB).
Definitions
- Strong electrolytes completely ionize in solution (e.g., NaCl, HCI).
- Weak electrolytes partially ionize in solution (e.g. lactic acid, ketoacids).
- Acid is a substance that can supply H+.
- Base is a substance that can take up H+ ions.
- Acetate is the conjugate base of acetic acid.
Dissociation Constant of a Weak Acid
- Weak acids or bases buffer against pH changes where the acid and conjugate base are comparable.
- A solution containing weak acid and its conjugate base acts as a buffer against added acid or base.
- Substances with a pK in the normal body pH range (7.40) possess a imidazole ring of the amino acid histidine or are phosphates.
- Imidazole in histidine has acidic and basic forms.
- The pKa of ≈7.0 is very close to the physiologic pH.
Titration Curve
- A titration curve plots the concentration of added strong acid/base against pH.
- Buffer value is the slope of the titration curve. It is used to calculate the titration curve for Imidazole.
- The curve is steepest at pH = pK.
- Little change in pH occurs for each mEq of added acid/base when pH is closest to pK.
- Titration curve is approximately linear between pH 6.5 and 7.5.
- Body fluid pH is accurately approximated by straight lines.
Titration With Imidazole
- If 4 mmol of HCl is added to 1 liter of imidazole solution, all added base combines with HIm+ and converts to Im+ water.
- Since the initial solution contains 10 mmol Im and 10 mmol HImt, basic form Im will decrease by 4 mmol to 6 mmol and the conjugate acid HImt will increase by 4 mmol to 14 mmol.
- [H+] concentration can be estimated from the table to be 2.33 nEq, giving a pH = 6.63.
- If 4 mmol of NaOH is added to 1 liter of the imidazole solution, it converts to Im+ water then HImt decreases by 4 mmol to 6 mmol and the conjugate base Im will increase by 4 mmol to 14 mmol.
- [H+] concentration can be estimated from the table to be 42.9 nEq, giving a pH = 7.37.
Body Acid-Base Review
- Large amounts of acid/base can be added to the body without lethal pH changes due to buffer substances.
- Most buffers are located intracellularly; this process is relatively slow.
- Intracellular buffers mainly consist of proteins and phosphates.
- Hemoglobin in red cells buffers acids/bases added to ECF and has a high histidine content: 36 histidines per hemoglobin tetramer. Histidine has the imidazole group and accounts for 90% of the blood's buffer value.
Hemoglobin as Buffer
-
High histidine content = 36 histidines in a tetramer
-
Most CO2 carried in blood is as HCO3 with
-
Most of the H+ is in the form of HImt in RBCS
-
All measurements of pH in blood are corrected to 100% saturation of Hgb with O2
-
ECF also includes buffers such as plasma proteins and phosphates.
-
Bone is a large sink for acids/bases, is a very slow buffer, and participates in chronic acidosis conditions.
-
Most CO2 carried by the blood is in the form of HCO3¯.
-
The H+ ions are carried in the form of HImt by histidines in hemoglobin.
-
Extracellular blood pH reflects intracellular pH.
-
Blood pH reflects pH in all parts of the body.
-
The HCO3-/CO2 buffer system is very important.
-
The pK=6.1 (not that close to physiologic).
-
Dual control comes from the lungs and the kidneys.
CO2 System
- Concentration of dissolved CO2 is [CO2]dis which is 0.03 mM/mmHg * pCO2
- pCO2 = 40 mmHg
- Dissolved CO2: all gases dissolve to some extent in water.
- Plasma [CO2]dis is proportional to the plasma pCO2
- Arterial blood is normally equilibrated with alveolar air.
- pCO2 is equal to the partial pressure of CO2 in alveolar air, normally 40 mmHg.
- [CO2]dis = 0.03 * 40 = 1.2 mM
- CO2 + H2O ↔ H+ + HCO3-
Henderson-Hasselbach Equation
- Doubling pCO2 form 40 to 80 mmHg increase the [HCO3¯] from 24 to 27 mEq, which is 3 mEq, and lowers the pH to 7.15.
- Henderson Hasselbach DOES NOT tell us the acid base disorder and is ALWAYS obeyed!
Buffering in Body – Using the Davenport Diagram
- The Davenport diagram is the section in the box of the titration curve for imidazole and can be used to assess buffering.
- The curve is steepest at neighborhood pH = pK.
- There is a little change in pH for each mEq of added acid/base when the pH is the closest to the pK.
- The titration curve is approximately linear between pH 6.5 and 7.5.
- The range of body fluid pH values compatible with life is less than one pH unit.
- Titration curves for body fluids are accurately approximated by straight lines.
- The HCO3 concentration is given on the Y-axis.
- The pH is given on the X-axis.
- Isobars are the curved lines, and they are constructed by drawing smooth curves through the points where pCO2 is constant.
- For measured pH, pCO2 and [HCO3¯], the third is calculated.
- Titration curves at fixed pCO2 is the pCO2 isobars and it is when Carbonic Acid/Bicarbonate Solution is added to fixed pCO2 values.
- Strong non-carbonic acid/base incrementally titrates to the solution.
Titration at Fixed pCO2
- Point O is normal for sea level humans = 40 mmHg
- The pCO2 is held constant at 40 mmHg
- Added HCl is buffered by NaHCO3.
- HCO3- decreases from 24 to 19 mM
- When very nearly all added HCl combines with NaHCO3 it forms CO2, H2O, and NaCl
- The pH drops to 7.3
- [HCO3] decreases by 5 mEq to a final value of 19 mM (mEq). The pH calculated from Henderson-Hasselbach is now 7.30. Point A is reached by adding 5 mEq of strong acid (HCI) to each liter of solution with the CO2 held constant at 40 mmHg.
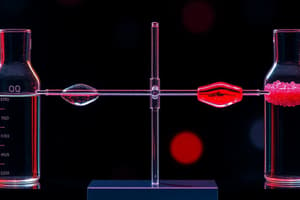
Titration of Body Fluid With H2CO3
- Where Hgb-Im represents titratable protein buffers and Hgb is on histidine with mostly imidazole.
- H2CO3 + Hgb-Im ↔ Hgb-Hlm+ + HCO3¯
- For each H+ buffered by Hab-Im a HCO3 ion appears
- = concentration of added H2CO3 gives The increase in [HCO3]
- The reaction of carbonic acid with buffers, the is When increasing dissolved CO2 gives increasing pCO2.
- The main buffering reaction, H2CO3 + Hgb-Im↔ Hgb-HImt + HCO3¯
Body Fluids of Non-Carbonic Acids
- The addition of strong non-carbonic acids/HCI is the combination of all added H+ ions with buffers.
- Acid in body fluids is buffered by the Im form of imidazole and the HCO3¯ to form carbonic acid
- Added carbonic acid is buffered by bicarbonate.
- Therefore, the change in [HCO3] does NOT represent the total amount of added acid.
Titration with Non-Carbonic Acid: Base Deficit
- Determination of the amount of added non-carbonic acid or base
- Point O the the initial condition where point A the condition after is added an unknown non-carbonic
- Most of the H+ ions combine with HCO3¯ to form CO2 and H2O.
- The remainder combine with Hgb and plasma proteins.
-
- L1 is the amount of HCl buffered by Hgb (HIm) and plasma proteins
- the A HCO3 of 2. L2 is the amount buffered by carbonic acid, from normal [HCO3] .
- 2 + L1 = base deficit
- The addition of a small amount of strong non-carbonic acid such as HCI to a buffered solution results in the combination of virtually all added H+ ions with the buffers.
- Acid is buffered by the im form of imidazole and the HCO3¯ to form carbonic acid
- Non carbonic acid is buffered by BOTH bicarbonate and hemoglobin
- Therefore, the change in HCO3 does NOT represent the total. amount added acid
Acid Base Compensation
-
Acid base disturbances are classified first by pH:
-
Acidemia – condition where pH < 7.40 (normal at sea level)
-
Alkalemia - condietion where pH > 7.40 (normal at sea level)
-
Then, sub-classified based on changes in carbonic acid or non-carbonic acid content:
-
Respiratory imbalance – changes in pCO2/carbonic acid due to changes in ventilation
-
▲ in volatile acid: pCO2 = measure of carbonic acid unbalance • pCO2 excess = respiratory acidosis • pCO2 deficit = respiratory alkalosis
-
Metabolic imbalance - changes in non-carbonic acid with base excess/deficit • ▲ in nonvolatile acid • Base deficit = metabolic acidosis • Base excess = metabolic alkalosis
-
If an arterial blood sample has abnormal pH, pCO2 and/or [HCO3-] values, then there is an acid base imbalance
-
The fact that the values are abnormal indicates a disturbance, but what is the SIZE of the disturbance?
-
the value of pCO2 is a good measure of the size of a carbonic acid imbalance but
-
[HCO3] is not a direct measure of the size of a non-carbonic acid imbalance
-
need to evaluate the base excess/base deficit
-
Normal Range: Acid-Base Values BOLD hexagon delineates the ranges of pH, pCO2 and [HCO3-] values in normal humans living near sea level with a body temperature of 37°C pH ≈ 7.35 to 7.45 (really more closely regulated to within 7.38 - 7.42 than can be shown on the graph easily) p CO2 ≈ 35 - 45 mmHg (as for pH, really more closely regulated to 37 - 42 mmHg) [HCO3-] ≈ 22 - 26 mEq
-
Normal values at sea level and 37°C are pH 7.40, HCO3- 24 mM, pCO2 40 mmHg
-
Obtain sample of arterial blood
-
Measure pH, pCO2 and [HCO3-]
-
Plot these values on the Davenport diagram
-
Make a diagnosis based on the position of the piont
-
If at all possible getting relevant history about the patient Focus on single acid-base disorder
Factors Affecting HCO3 Reabsorption
- It will be good to review the factors affecting reabsorption at that time
- CO2 + H2O ↔ H2CO3 ↔ H+ + HCO3-
- Carbonic anhydrase (CA) activity: ↓carbonic anhydrase activity→
- ↓H+ secretion →↓ reabsorption of HCO3: Partial pressure (PCO₂): ↓PCO2→↓ HCO3- reabsorption
- Amount filtered HCO3↑ ↑HCO3filtered→HCO3 reabsorption
- Amounts of filtered/secreted buffers (distal): and that be protonated to and H2PO
Compensation
- Respiratory Acidosis (Hypercapnia): Carbonic Acid Excess
- [H+] * [HCO3- ] = 0.03 Ka pCO2
- Normal
- Uncompensated
- Compensated (physiologic response)
- A disorder is when high and low pH is move to higher isobar.
Respiratory Alkalosis
- Compensation is when kidney increases excretion will manifest as further increase in along the same isobar/Renal compensated
Malfunctions Causing Respiratory Acidosis (Hypercapnia)
- Pulmonary disease: Asthma, COPD
- Neuromuscular disorders: Myasthenia gravis, Poliomyelitis,Spinal cord lesions
- Restricted thoracic movement: Obesity, Arthritis
- Chemoreceptor depressants: Anesthetics, Sedatives, Narcotics
Acute vs Chronic Respiratory Acidosis (or Hypercapnia)
- [H+] = 0.03 Ka
- Acutely the pCO2 increased and over time the compensatory physiologic response
Respiratory Alkalosis: Carbonic Acid Deficit
- is a deficit carbonic acid (content- the elevated
- The decrease CO2 decreased
- Cells increase production
- The kidney + (acid), -is
Malfunctions Causing Respiratory Alkalosis (Hypocapnia)
- The primary problem is a deficit carbonic acid
- Initial/ Low
- Decreases the + + Cell will ncrease production thekidney then
Metabolic Acidosis
- The of in
- a H2CO3 a. ketodacids 2
- The kidney be
- increase pH .
- to with
Malfunctions Causing Metabolic Alkalosis vomiting
Overview/Summary
- primary = metabolic acidosis the pCO2 high then with primary/
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.