Podcast
Questions and Answers
What should be done to assess the visual fields of a patient?
What should be done to assess the visual fields of a patient?
- Cover your eye opposite the patient’s closed eye and move your fingers into their peripheral vision. (correct)
- Keep both eyes open and ask the patient to close theirs while inspecting.
- Simultaneously point at the patient's nose and ask them to follow your finger.
- Cover the patient's eye opposite to yours and move your arm in one direction only.
What is the primary focus when inspecting the external ear?
What is the primary focus when inspecting the external ear?
- Look for symmetry with the patient's eyes closed.
- Listen for sounds while palpating the ear.
- Inspect and palpate the external ear systematically. (correct)
- Examine the ear canal for wax only.
Which technique is used to assess nasal patency?
Which technique is used to assess nasal patency?
- Palpate the sinuses while the patient breathes normally.
- Tilt the patient's head back and visualize the throat.
- Occlude one nostril and ask the patient to inhale and exhale. (correct)
- Open the mouth and look for swelling.
What is an abnormal finding when assessing the nasal mucosa?
What is an abnormal finding when assessing the nasal mucosa?
How should the patient's head be positioned during sinus palpation?
How should the patient's head be positioned during sinus palpation?
What indicates a normal nasal mucosa during inspection?
What indicates a normal nasal mucosa during inspection?
What should be checked during examination of the external ear?
What should be checked during examination of the external ear?
What common misinterpretation may occur when assessing visual fields?
What common misinterpretation may occur when assessing visual fields?
What should be assessed in the nares during the nasal examination?
What should be assessed in the nares during the nasal examination?
What is an important step before palpating the sinuses?
What is an important step before palpating the sinuses?
Flashcards are hidden until you start studying
Study Notes
Adventitious Breath Sounds
- Abnormal lung sounds arise from air flow through moisture, mucus, or narrowed airways.
- Sudden opening of collapsed alveoli can also cause abnormal breath sounds.
- Bronchial sounds: high-pitched, harsh, predominant on expiration, heard over larynx and trachea.
- Bronchovesicular sounds: moderate blowing sounds with equal inspiration and expiration, found over the mainstem bronchus.
Skin Conditions and Symptoms
- Cyanosis: Bluish discoloration indicating insufficient oxygen; assessed differently in light and dark skin.
- Diaphoresis: Excessive sweating with moist skin.
- Ecchymosis: Subcutaneous blood collection leading to purple discoloration.
- Edema: Excess tissue fluid causing swelling; may present as pitting edema if indentations remain after pressure.
- Jaundice: Yellowish skin due to elevated bilirubin, prevalent in liver and gallbladder diseases; first seen in sclera.
Anemias and Pallor
- Pallor: Skin paleness from decreased blood or hemoglobin; may appear as ashen or yellow in darker skin tones.
- Petechiae: Small hemorrhagic spots, requiring assessment for location, color, and size.
Types of Health Assessments
- Comprehensive Health Assessment: Initial thorough evaluation including health history and physical examination to establish baseline data.
- Emergency Health Assessment: Rapid focused assessment during life-threatening situations, prioritizing airway, breathing, and circulation.
- Follow-Up Assessment: Conducted at regular intervals to monitor changes in health conditions and the effectiveness of interventions.
Inspection and Assessment Techniques
- Auscultation: Listening to body sounds; involves proper positioning and stethoscope use.
- BMI Calculation: Determines nutritional status and obesity risk via weight-to-height ratio.
- Palpation: Touch to assess skin temperature, turgor, texture, and underlying structures.
- Percussion: Tapping body parts to produce sounds that reveal tissue conditions.
Additional Health Notes
- Turgor: Skin elasticity assessment; decreased turgor indicates dehydration or aging.
Skin Lesions and Conditions
- Lesions typically should not change color, have a diameter of less than 6mm, regular borders, and symmetry.
- Chloasma (Melasma): Brown patches on the skin, often associated with pregnancy.
- Impetigo: Highly contagious bacterial skin infection with honey-colored crusts.
- Melanoma: Skin cancer characterized by asymmetrical, irregularly bordered moles with color variation.
Physical Characteristics to Assess
- Warning signs of melanoma: Asymmetry, uneven borders, varied colors, diameter over 6mm, and any evolving traits.
- Hyperemia: Reddened skin due to increased blood flow, should blanch under pressure.
Common Skin Issues
- Tinea Capitis: Common fungal infection with a ring-like rash.
- Acne: Clogged pores leading to inflamed lesions.
- Vitiligo: Skin depigmentation resulting in whitish patches.
Growth and Development Considerations
- Comprehensive assessments throughout life involve evaluating cognitive, psychosocial, and emotional development alongside physical growth.### Cultural Considerations and Sensitivity
- Cultural assessment is vital in health evaluations and includes questions to gather cultural data about patients, families, and caregivers.
Patient Preparation
- Physiological needs: Address pain and stamina affected by age or illness.
- Psychological needs: Acknowledge anxiety regarding assessments.
Environmental Preparation
- Privacy and respect are crucial during health assessments.
- Utilize separate examination rooms in outpatient settings for assessments.
Nurse’s Role in Diagnostic and Laboratory Testing
- Diagnostic tests provide essential health information and become part of total health assessment.
- Nurses facilitate the process, prepare patients, and educate them about procedures and tests.
Health History
- A comprehensive health history helps develop a patient profile and identify health issues.
- Key components of health history include:
- Biographical data: Collect demographic and personal details to establish risk factors.
- Reason for seeking healthcare: Record patient’s statements in their own words.
- Present health history: Detail current symptoms, including onset, location, and previous treatments.
- Past health history: Gather information on previous illnesses, surgeries, and allergies.
- Family health history: Identify genetic risks and exposure to communicable diseases.
- Functional health: Assess patients’ ability to perform activities of daily living (ADLs) and instrumental activities of daily living (IADLs).
- Review of systems: Ask targeted questions across body systems to uncover health concerns.
Physical Assessment
- A systematic physical assessment involves objective information collection, typically in a head-to-toe or systems-based approach.
- Adjustments in assessment may be necessary based on patient condition and constraints.
Preparing for a Physical Examination
- Ensure patient comfort prior to examination using effective communication.
- Make sure all assessment equipment is accessible, clean, and functioning properly.
Key Assessment Equipment
- Thermometer: Measures body temperature.
- Blood pressure devices (oscillometric or sphygmomanometer): Necessary for blood pressure evaluation.
- Scale: Assesses weight and height, with special scales for limited mobility patients.
- Flashlight or penlight: Used for detailed inspections (e.g., mouth, eyes).
- Stethoscope: Auscultates heart, lung, and abdominal sounds.
- Metric tape measure and ruler: Measures body circumferences and wounds.
- Eye chart (Snellen chart): Screens for vision clarity.
Techniques of Physical Assessment
- Inspection: Careful visual observation of patient appearance and behavior.
- Palpation: Using touch to assess skin characteristics and internal structures.
- Percussion: Tapping to produce sounds, providing information on tissue characteristics.
- Auscultation: Listening for internal sounds, noting pitch, loudness, quality, and duration.
Conducting a Physical Assessment
- General survey includes assessing appearance, behavior, and vital signs.
- Health history: Identify altered health risks (e.g., weight changes, pain, sleep problems).
- Appearance and behavior observation: Offers insight into overall health and cognitive processes.
- Vital signs: Establish baselines for identifying health issues.
Assessing Integument
- Skin, hair, and nails reflect overall health status; essential for skin cancer evaluation.
- Inspect for color changes (e.g., erythema, cyanosis, jaundice, pallor) and health implications.
Skin Color Assessment
- Erythema: Redness due to blood vessel dilation; indicative of trauma or infection.
- Cyanosis: Bluish hue reflecting inadequate oxygenation; observed in lips and extremities.
- Jaundice: Yellow discoloration from elevated bilirubin, signals liver issues.
- Pallor: Pale skin due to reduced oxygenation; affects the face and mucous membranes.
These detailed elements of the health assessment process illustrate the critical role of nurses in evaluating and supporting patient health through sensitive and thorough practices.### Skin Inspection
- Pallor in dark-skinned individuals appears as an ashen gray or yellow tinge.
- Inspect for vascularity, bleeding, or bruising; indicators of cardiovascular, hematologic, or liver dysfunction.
- Ecchymosis represents subcutaneous blood collection, leading to purplish discoloration; petechiae are small hemorrhagic spots due to capillary bleeding.
- Assess lesions and wounds for size, shape, depth, location, drainage, and odor; types include bruises, scratches, cuts, and insect bites.
- Rashes need evaluation based on type, size, elevation, color, and presence of drainage or itching.
- Document specific surface areas affected and evaluate body piercings and tattoos.
Skin Characteristics
- Normal skin is warm and dry; temperature increase with moisture may indicate fever.
- Skin texture ranges from smooth and soft to rough and dry; dehydration results in dry, loose, and wrinkled skin.
- Diaphoresis indicates excessive sweating; skin turgor denotes skin fullness and elasticity, assessed via skin fold test.
- Decreased skin turgor indicates dehydration and slow fold return; normal changes in older adults may present as decreased elasticity.
- Edema is characterized by swelling and taut skin, with pitting edema showing lasting indentations after pressure.
Nail Inspection
- Nails should be convex, smooth, and follow the finger's natural curve, with a normal angle of about 160 degrees.
- Abnormalities include infections, separation of nail plates, increased brittleness, and clubbing linked to reduced oxygen levels.
Hair and Scalp Assessment
- Assess hair for color, texture, and distribution; hair should be resilient and equally distributed.
- Abnormal findings include balding (alopecia) and excess body hair (hirsutism), with hair loss potentially resulting from various medical issues.
- Scalp inspection for color, dryness, and lice; nits are distinguishable by their attachment to hair shafts.
Age-Related Skin Variations
- Infants may display jaundice, milia, and lanugo; skin is smooth and thin at birth.
- Older adults typically show wrinkles, dryness, senile keratosis, age spots, and hair changes like graying or brittleness.
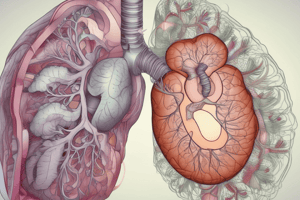
Head and Neck Assessment
- Assess the skull, face, eyes, ears, nose, mouth, trachea, thyroid gland, and lymph nodes.
- Pay attention to health history for headaches or dizziness; consider smoking cessation in the care plan.
- Physical examination should assess cranial bone structure and lymph node conditions.
Eye Inspection
- Use a penlight and an eye chart for assessing eye structures, visual acuity, and extraocular movements.
- Pupillary reaction involves checking for constriction upon light exposure; accommodation evaluates response to distance changes.
- Convergence is assessed by having the patient follow a finger towards their nose.
Ear Inspection
- Inspect the external ear visually and through palpation while assessing hearing and sound conduction.
Nose Examination
- Inspect the external nose and nares; assess patency by occluding nostrils.
- Examine nasal mucosa for hydration and lesions; normal mucosa is moist and darker than oral mucosa.
- Swelling, bleeding, or discharge may indicate allergies or infections.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.