Podcast
Questions and Answers
How do the diaphragm and intercostal muscles contribute to ventilation?
How do the diaphragm and intercostal muscles contribute to ventilation?
- Diaphragm contraction increases thoracic volume, and intercostal muscles assist in expanding and contracting the chest cavity. (correct)
- Intercostals initiate the breathing process, and the diaphragm regulates the depth of respiration.
- The diaphragm primarily controls the speed of airflow, while intercostals adjust airway diameter.
- The diaphragm and intercostals are responsible for gas exchange in the alveoli.
During quiet respiration, which muscles are primarily responsible for the movement of air?
During quiet respiration, which muscles are primarily responsible for the movement of air?
- Only the diaphragm
- Abdominal muscles
- Intercostal muscles only
- Diaphragm and intercostal muscles (correct)
Which aspect of lung physiology does smooth muscle primarily influence?
Which aspect of lung physiology does smooth muscle primarily influence?
- Regulation of alveolar surface tension
- Adjustment of airflow via changes in airway diameter (correct)
- Maintenance of lung elasticity
- Control of the rate of gas exchange
Which of the following muscles are recruited during forced expiration?
Which of the following muscles are recruited during forced expiration?
What is the effect on thoracic volume when the diaphragm contracts?
What is the effect on thoracic volume when the diaphragm contracts?
What crucial function do the intercostal muscles serve during inhalation?
What crucial function do the intercostal muscles serve during inhalation?
During normal expiration, which of the following processes occurs?
During normal expiration, which of the following processes occurs?
What is the role of the 'braking action' during expiration?
What is the role of the 'braking action' during expiration?
What physiological effect does abdominal pressure influence?
What physiological effect does abdominal pressure influence?
What is the Valsalva maneuver, and when is it typically employed?
What is the Valsalva maneuver, and when is it typically employed?
Which of the following best describes the primary function of the ventral respiratory group (VRG)?
Which of the following best describes the primary function of the ventral respiratory group (VRG)?
How do the inspiratory (I) and expiratory (E) neurons within the ventral respiratory group (VRG) interact to control breathing?
How do the inspiratory (I) and expiratory (E) neurons within the ventral respiratory group (VRG) interact to control breathing?
Which of the following describes the role of the dorsal respiratory group (DRG) in respiratory control?
Which of the following describes the role of the dorsal respiratory group (DRG) in respiratory control?
What is the primary function of the pontine respiratory group (PRG)?
What is the primary function of the pontine respiratory group (PRG)?
How do central chemoreceptors respond to changes in the cerebrospinal fluid (CSF)?
How do central chemoreceptors respond to changes in the cerebrospinal fluid (CSF)?
Peripheral chemoreceptors are located in the carotid and aortic arteries. Which aspects of blood chemistry do these receptors primarily monitor?
Peripheral chemoreceptors are located in the carotid and aortic arteries. Which aspects of blood chemistry do these receptors primarily monitor?
What is the primary role of stretch receptors in the lungs?
What is the primary role of stretch receptors in the lungs?
How do irritant receptors in the respiratory system respond to harmful stimuli?
How do irritant receptors in the respiratory system respond to harmful stimuli?
How does voluntary control of breathing override the automatic controls?
How does voluntary control of breathing override the automatic controls?
What is the primary determinant of airflow?
What is the primary determinant of airflow?
According to Boyle's Law, how does an increase in lung volume affect intrapulmonary pressure during inhalation?
According to Boyle's Law, how does an increase in lung volume affect intrapulmonary pressure during inhalation?
How is the pressure gradient that drives airflow into the lungs established during inhalation?
How is the pressure gradient that drives airflow into the lungs established during inhalation?
What is the definition of pneumothorax?
What is the definition of pneumothorax?
How does pneumothorax affect the pressure dynamics within the thoracic cavity, and what is the consequence?
How does pneumothorax affect the pressure dynamics within the thoracic cavity, and what is the consequence?
What is the effect of bronchodilation on airway resistance?
What is the effect of bronchodilation on airway resistance?
Which of the following factors can directly cause bronchoconstriction?
Which of the following factors can directly cause bronchoconstriction?
How does increased pulmonary compliance affect the effort required for breathing?
How does increased pulmonary compliance affect the effort required for breathing?
What is the effect of scar tissue on pulmonary compliance?
What is the effect of scar tissue on pulmonary compliance?
How does surface tension affect the alveoli, and how is this effect counteracted?
How does surface tension affect the alveoli, and how is this effect counteracted?
What is the role of surfactant in the alveoli?
What is the role of surfactant in the alveoli?
What is anatomical dead space?
What is anatomical dead space?
Which of the following is the best definition of physiological dead space?
Which of the following is the best definition of physiological dead space?
What is the significance of residual volume in the lungs?
What is the significance of residual volume in the lungs?
What is the definition of Alveolar Ventilation Rate (AVR)?
What is the definition of Alveolar Ventilation Rate (AVR)?
How does residual volume affect gas exchange in the alveoli?
How does residual volume affect gas exchange in the alveoli?
In the context of alveolar ventilation, why might reduced gas exchange cause respiratory distress?
In the context of alveolar ventilation, why might reduced gas exchange cause respiratory distress?
Flashcards
Respiratory cycle
Respiratory cycle
A repetitive cycle of inspiration (inhaling) and expiration (exhaling).
Smooth muscle
Smooth muscle
Adjusts airway diameter in lungs affecting airflow speed. Does not create airflow.
Recruitment of muscles
Recruitment of muscles
Muscles including the diaphragm and intercostals, help expand/contract the chest cavity changing pressure.
Diaphragm
Diaphragm
Signup and view all the flashcards
Intercostals role
Intercostals role
Signup and view all the flashcards
Intercostals (air)
Intercostals (air)
Signup and view all the flashcards
Erector spinae
Erector spinae
Signup and view all the flashcards
Pectoralis major/minor function
Pectoralis major/minor function
Signup and view all the flashcards
Normal Expiration
Normal Expiration
Signup and view all the flashcards
Braking action role
Braking action role
Signup and view all the flashcards
Abdominal pressure influence
Abdominal pressure influence
Signup and view all the flashcards
Diaphragm depression
Diaphragm depression
Signup and view all the flashcards
Valsalva maneuver
Valsalva maneuver
Signup and view all the flashcards
Ventral respiratory group (VRG)
Ventral respiratory group (VRG)
Signup and view all the flashcards
Inspiratory (I) neurons function
Inspiratory (I) neurons function
Signup and view all the flashcards
Expiratory (E) neurons function
Expiratory (E) neurons function
Signup and view all the flashcards
Eupnea rate
Eupnea rate
Signup and view all the flashcards
Dorsal respiratory group (DRG) function
Dorsal respiratory group (DRG) function
Signup and view all the flashcards
Pontine Respiratory Group (PRG) function
Pontine Respiratory Group (PRG) function
Signup and view all the flashcards
Central chemoreceptors
Central chemoreceptors
Signup and view all the flashcards
Peripheral chemoreceptors
Peripheral chemoreceptors
Signup and view all the flashcards
Stretch receptors
Stretch receptors
Signup and view all the flashcards
Inflation reflex
Inflation reflex
Signup and view all the flashcards
Irritant receptors function
Irritant receptors function
Signup and view all the flashcards
Voluntary Control origin
Voluntary Control origin
Signup and view all the flashcards
Airflow determinants
Airflow determinants
Signup and view all the flashcards
Atmospheric pressure
Atmospheric pressure
Signup and view all the flashcards
Boyle's Law
Boyle's Law
Signup and view all the flashcards
Air flow concentration
Air flow concentration
Signup and view all the flashcards
Intrapulmonary pressure
Intrapulmonary pressure
Signup and view all the flashcards
Pneumothorax
Pneumothorax
Signup and view all the flashcards
Diameter of bronchioles
Diameter of bronchioles
Signup and view all the flashcards
Pulmonary Compliance definition
Pulmonary Compliance definition
Signup and view all the flashcards
Surfactant function
Surfactant function
Signup and view all the flashcards
Anatomical dead space
Anatomical dead space
Signup and view all the flashcards
Physiological dead space
Physiological dead space
Signup and view all the flashcards
Alveolar Ventilation Rate (AVR)
Alveolar Ventilation Rate (AVR)
Signup and view all the flashcards
Residual volume
Residual volume
Signup and view all the flashcards
Study Notes
Mechanics of Breathing and Neural Control
- Chapter 22 focuses on the mechanics of breathing and neural control of the respiratory system.
Objectives
- Describe the roles of muscles in breathing.
- Identify brainstem centers that control breathing.
- Explain how pressure gradients influence breathing.
- Explain how pressure gradients are produced.
- Describe sources of respiratory resistance.
- Explain the significance of dead space to ventilation.
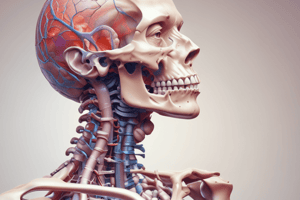
Pulmonary Ventilation
-
Pulmonary ventilation involves the repetitive cycle of inspiration (inhaling) and expiration (exhaling).
-
One complete breath (in and out) is termed a respiratory cycle.
-
The only muscle in the lungs is smooth muscle in the walls of the bronchioles. This muscle adjusts the diameter of the airway and affects the speed of airflow; it does not create airflow.
- Blood vessels
-
The recruitment of muscles, including the diaphragm and intercostal muscles, help to expand and contract the chest cavity, which in turn changes the pressure inside the lungs and drives air in and out.
-
Diaphragm
- The diaphragm is the prime mover, responsible for producing about 2/3 of airflow.
- Stimulation of the diaphragm pulls it down, increasing thoracic volume.
- Relaxation of the diaphragm results in recoil, decreasing thoracic volume.
Other Muscles (non-diaphragm)
- Intercostals
- The intercostals stiffen the thoracic cage during inhalation to prevent collapsing and pull ribs upwards, expanding the cavity.
- Involved in transverse and anteroposterior dimension changes
- transverse dimension: lateral expansion of the thoracic cavity, helping to create more space for the lungs to fill with air
- anteroposterior dimension: forward and backward expansion of the thoracic cavity, allowing the lungs to expand further, facilitating a greater volume for air intake
- Contribute about 1/3 of airflow.
- Intercostals also assist with forced expiration by pushing ribs downward.
- Accessory Muscles
- usually involved with forced breathing.
- Erector Spinae arches the back.
- Pectoralis major and minor lift the ribs.
- erector spinae and pectoralis major/minor increases the volume of the chest cavity
- Rectus abdominis and other abdominal muscles aid in breathing.
Normal Expiration
- Normal expansion is an energy-saving passive process achieved by:
- Lung elasticity.: these structures recoil when the muscles relax
- Bronchial tree
- Rib attachments
- Tendons of muscles
- Lung elasticity.: these structures recoil when the muscles relax
- Braking action - occurs during expiration.
- the only muscular effort involved in normal expiration
- Muscles gradually relax, preventing the lungs from recoiling too suddenly.
- This makes a smooth transition from inspiration to expiration.
Abdominal Pressure
- Thoracic pressure can influence the abdomen.
- Diaphragm depression raises abdominal pressure to help expel contents of abdominal organs.
- Examples: urination, defecation, childbirth, and vomiting.
- The Valsalva maneuver involves taking a deep breath, holding it, and contracting abdominal muscles to push the organ contents out.
Brain Respiratory Centers
1. Ventral Respiratory Group (VRG)
- The location of the VRG is in the medulla oblongata.
- VRG uses a reverberating circuit.
- Inspiratory (I) neurons stimulate the phrenic nerve and costal nerves, which contract the diaphragm and intercostal muscles
- Expiratory (E) neurons inhibit I neurons, leading to recoil.
- The I circuit issues signals to the spinal cord (SC) integration center to the phrenic nerve, which leads to the diaphragm and the intercostal nerves, which lead to external intercostal muscles. Contraction of these muscles enlarges the thoracic cage and causes inspiration.
- Eupnea: normal quiet breathing that operates at 12 breaths/min.
2. Dorsal Respiratory Group (DRG)
- Present and active during quiet breathing
- Located in the medulla oblongata.
- DRG activity modifies the basic respiratory rhythm set by the VRG.
- This is done by integration of sensory information from chemoreceptors (medulla oblongata, arteries), stretch receptors (airways), and brainstem centers for emotional pathways.
- DRG output affects the VRG, changing the respiratory rhythm to adapt to varying conditions.
3. Pontine Respiratory Group (PRG)
- Located on each side of the pons.
- PRG receives sensory input from the hypothalamus, limbic system, and cerebral cortex.
- PRG relays information and output to the VRG and DRG centers in the medulla oblongata.
- PRG regulates short/long and shallow/deep breaths and adapts to conditions like sleep, exercise, and emotions (breathing during crying, laughing, etc.)
Input to Respiratory Centers
Central Chemoreceptors
- Brainstem neurons that monitor CSF pH.
Peripheral Chemoreceptors
- Peripheral chemoreceptors are located in carotid arteries (via glossopharyngeal nerves) and aortic arteries (via vagus nerves).
- Peripheral chemoreceptors monitor oxygen and carbon dioxide levels and pH in the blood.
- Information is then sent into the DRG, triggering changes in rate and depth of breathing to enhance oxygen intake, expel more carbon dioxide from the body, or restore normal acid-base balance.
Stretch Receptors
- Stretch receptors are located in smooth muscle of the visceral pleura and the bronchi & bronchioles.
- Stretch receptors respond to inflation of the lungs.
- Signals are sent via vagus nerves to the DRG.
- The inflation reflex is triggered by excessive inflation. In this situation, the I neurons are inhibited and stop inhalation
- This protective somatic reflex strongly inhibits the I neurons, stopping inspiration and is important during vigorous exercise or taking deep breaths
- Inflation Reflex in Infants
- In infants, Inflation reflex may be a normal mechanism of transition from inspiration to expiration, but after infancy it is activated only by extreme stretching of the lungs
Irritant Receptors
- Irritant receptors are nerve endings located among epithelial cells.
- They respond to smoke, dust, pollen, fumes, cold, and mucus levels.
- The signals are sent via the vagus nerve signal to the DRG.
- The DRG signals respiratory and bronchial muscles.
- This results in reflexes like bronchoconstriction, shallower breathing, breath-holding (apnea), or coughing.
- The DRG signals respiratory and bronchial muscles.
Voluntary Control
- Voluntary control originates in the cerebral motor cortex, which sends signals via the corticospinal tract to spinal cord (SC) integration centers, bypassing brainstem centers.
- It is impossible to hold one's breath until death. Holding your breath raises the CO2 level of the blood until the brainstem overrides you by forcing the body to breathe.
What Determines Airflow?
- Pressure and resistance.
Pressure, Airflow
-
Atmospheric pressure is the weight of the air above us, while intrapulmonary pressure is the pressure within the lungs.
-
Boyle's Law drives inspiration.
- Pressure of gas is inversely proportional to volume.
-
Air flows down concentration (pressure) gradient
-
During inhalation:
- Intrapulmonary pressure is less than atmospheric pressure, allowing air to flow into the lungs.
-
e.g. Inspiration
- Ribs and pleura expand outward, which causes pressure to decrease within the alveoli (Boyle's Law).
- Air flows from high to low (pressure gradient) into alveoli
-
If the lungs contain a quantity of gas and lung volume increases, their internal pressure falls.
-
Conversely, if lung volume decreases, intrapulmonary pressure rises
Pneumothorax
- The presence of air in the pleural cavity.
- This happens because the thoracic wall is punctured.
- Inspiration sucks air through the puncture wound, which causes pleurae to separate.
- Negative interpulmonary pressure can't be established, so the lung collapses.
Resistance to Airflow
- Resistance to airflow is affected by:
- Diameter of bronchioles: dilation or constriction.
- Pulmonary Compliance: How easily the lungs expand.
Bronchiole Diameter
- Bronchiole diamater is reduced (bronchoconstriction) or expanded (bronchodilation) and can be controlled by hormones like epinephrine & norepinephrine, which stimulates bronchodilation, or histamine, acetylcholine, cold temperature, & irritants, which stimulates bronchoconstriction.
- Many people have suffocated from extreme bronchoconstriction brought on by anaphylactic shock or asthma
Pulmonary Compliance
- High compliance (flexibility) causes decreased resistance and vice versa.
- Diseases such as tuberculosis and black lung disease cause scar tissue, which stiffens the lungs and reduces this compliance.
Surface Tension
- The thin water layer on the respiratory membrane creates potential for maintaining ventilation.
Water Attraction
- Water is attracted to other water molecules by hydrogen bonds, creating surface tension.
- Without surfactant, water attraction can cause walls of small airways (bronchioles and alveolar ducts) to collapse
Surfactant
- Surfactant is a solution to this problem that reduces surface tension.(examples: soap and detergent)
- It does this by disrupting H-bonds.
- Deep breathing spreads surfactant in smaller airways.
- Patients recovering from surgery are encouraged to breath deeply even in order to promote this spreading and prevent the lungs from collapsing.
Alveolar Ventilation
- Alveolar ventilation involves the actual movement of air into and out of alveoli.
- Key Features:
- Anatomic Dead Space: Conducting zone where no gas exchange occurs (About 150 ml of inhaled air.)
- Physiological Dead Space: Total dead space (includes pathological dead space)
- Alveolar Ventilation Rate (AVR): Rate at which air moves in and out of the alveoli
- Resistance: high at terminal bronchioles.
- How does gas move into and out of the alveoli?
- oxygen completes its journey to the alveoli, and carbon dioxide leaves them by simple diffusion
- Residual volume
- the lungs never completely empty during expiration
- the leftover air is called residual volume
- it cannot be exhaled even with maximum effort
- It gets mixed with fresh incoming air and takes 18 average breaths to replace all the pulmonary air.
- result if you could exhale it?
- decreased gas exchange
- potentially collapsed lungs
- increase the workload of breathing
- causing respiratory distress
- the lungs never completely empty during expiration
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.