Podcast Beta
Questions and Answers
What occurs when Na channels open in a neuron?
What is the threshold potential required to initiate an action potential in neurons?
During hyperpolarization, what is the approximate membrane potential?
Which stage of the sodium channels prohibits Na movement?
Signup and view all the answers
What is the main role of the Na/K pump during the action potential process?
Signup and view all the answers
Which system is characterized by using chemical messengers that travel through the bloodstream?
Signup and view all the answers
How does the speed of reaction in the endocrine system compare to that of the nervous system?
Signup and view all the answers
What is the primary function of the nervous system?
Signup and view all the answers
In terms of distance of action, what distinguishes the nervous system from the endocrine system?
Signup and view all the answers
Which of the following correctly describes the anatomical arrangement of the endocrine system?
Signup and view all the answers
What is the primary role of the sympathetic nervous system?
Signup and view all the answers
Which part of the neuron is primarily responsible for receiving signals from other cells?
Signup and view all the answers
What is the main function of the myelination of axons?
Signup and view all the answers
What type of neuron carries sensory messages into the central nervous system?
Signup and view all the answers
What does the axon hillock do in a neuron?
Signup and view all the answers
Which type of glial cell is responsible for myelination in the central nervous system?
Signup and view all the answers
What is the role of the absolute refractory period in action potentials?
Signup and view all the answers
What defines visceral stimuli?
Signup and view all the answers
During which phase is a stronger stimulus required to initiate an action potential?
Signup and view all the answers
Which of the following is NOT part of a neuron?
Signup and view all the answers
What process gives the illusion of action potentials 'jumping' between nodes of Ranvier?
Signup and view all the answers
Which of the following neurotransmitters is an inhibitory neurotransmitter?
Signup and view all the answers
What is the primary function of neuroactive peptides?
Signup and view all the answers
Which of the following is NOT classified as an amino acid neurotransmitter?
Signup and view all the answers
What is the first step in the process of chemical signaling between neurons?
Signup and view all the answers
Catecholamines are derived from which amino acid?
Signup and view all the answers
What happens to PCO2 and pH when the respiratory rate (RR) is increased?
Signup and view all the answers
What is the primary method of regulation performed by the kidneys in pH balance?
Signup and view all the answers
In metabolic acidosis, which of the following is a possible cause?
Signup and view all the answers
Which parameter is typically low in respiratory acidosis?
Signup and view all the answers
What can cause respiratory alkalosis?
Signup and view all the answers
How does the body compensate during metabolic alkalosis?
Signup and view all the answers
Which buffer system operates intracellularly and extracellularly?
Signup and view all the answers
How does renal failure contribute to metabolic acidosis?
Signup and view all the answers
Which pH disturbance is characterized by high pH and normal PCO2?
Signup and view all the answers
What effect does an increased respiratory rate have on blood carbon dioxide levels?
Signup and view all the answers
Identify the role of the axon in a neuron.
Signup and view all the answers
What primarily determines the speed of action potentials in myelinated neurons?
Signup and view all the answers
What characterizes the autonomic nervous system's sympathetic division?
Signup and view all the answers
What is the function of Schwann cells in the peripheral nervous system (PNS)?
Signup and view all the answers
In which part of a neuron does the action potential typically begin?
Signup and view all the answers
What type of neuron connects sensory neurons to motor neurons?
Signup and view all the answers
Which structure in a neuron is responsible for synthesizing neurotransmitters?
Signup and view all the answers
What is the primary role of the autonomic nervous system?
Signup and view all the answers
What is the main purpose of oxygen in oxidative phosphorylation?
Signup and view all the answers
Which transport mechanism requires energy to move substances against their concentration gradient?
Signup and view all the answers
What describes coagulative necrosis?
Signup and view all the answers
What type of cell injury can recover if stress is relieved early?
Signup and view all the answers
In which cellular location does glycolysis occur?
Signup and view all the answers
What adaptation might occur due to persistent stress on a cell?
Signup and view all the answers
Which type of necrosis results in tissue appearing liquefied?
Signup and view all the answers
What is the ATP yield during oxidative phosphorylation?
Signup and view all the answers
What is a characteristic change observed during pyknosis?
Signup and view all the answers
Which transport mechanism does NOT require energy?
Signup and view all the answers
What distinguishes the absolute refractory period from the relative refractory period?
Signup and view all the answers
Which neurotransmitter is considered a generic inhibitory neurotransmitter?
Signup and view all the answers
What role do neuroactive peptides play in neurotransmission?
Signup and view all the answers
Which type of conduction provides the illusion of action potentials jumping between nodes of Ranvier?
Signup and view all the answers
Which neurotransmitter is derived from the amino acid tyrosine?
Signup and view all the answers
Which statement is true regarding the communication at synapses?
Signup and view all the answers
Which neurotransmitter is specifically classified as an excitatory amino acid neurotransmitter?
Signup and view all the answers
What is the main function of sodium channels during the absolute refractory period?
Signup and view all the answers
What is the primary function of the Na/K pump in relation to resting membrane potentials?
Signup and view all the answers
Which ion movement primarily contributes to the resting membrane potential being negative?
Signup and view all the answers
How does the Nernst equation relate to ion equilibrium in neurons?
Signup and view all the answers
When neurotransmitters bind to dendrites, what effect does this have on ion channels?
Signup and view all the answers
What does the equilibrium potential for an ion reflect?
Signup and view all the answers
Which ion's movement into the cell is primarily responsible for depolarization during action potentials?
Signup and view all the answers
What is the net resting membrane potential in a neuron at rest?
Signup and view all the answers
What does the term 'electrostatic gradient' refer to in the context of ion movement?
Signup and view all the answers
What defines caseous necrosis?
Signup and view all the answers
Which step is NOT part of the apoptosis process?
Signup and view all the answers
Which mechanism causes hypoxic injury to cells?
Signup and view all the answers
What is the most common free radical produced as a byproduct of metabolism?
Signup and view all the answers
Which adaptation refers to an increase in cell number while cell size remains the same?
Signup and view all the answers
Which condition is commonly associated with lipid accumulation in liver cells?
Signup and view all the answers
Which of the following is NOT a trigger for apoptosis?
Signup and view all the answers
What is a characteristic feature of dysplasia?
Signup and view all the answers
What common injury can lead directly to saponification during cell death?
Signup and view all the answers
What effect does increased intracellular calcium have during hypoxic injury?
Signup and view all the answers
Which adaptation occurs with decreased functional demands on cells?
Signup and view all the answers
Which change involves the replacement of ciliated epithelium with simple squamous cells?
Signup and view all the answers
What is the primary function lost in cells undergoing dysplasia?
Signup and view all the answers
What is the primary factor that affects the specificity of action in the endocrine system?
Signup and view all the answers
How does the duration of action differ between the nervous system and endocrine system?
Signup and view all the answers
Which characteristic of the nervous system allows for rapid coordination of precise reactions?
Signup and view all the answers
Which of the following statements correctly describes the relationship between the nervous system and endocrine system?
Signup and view all the answers
In which area does the peripheral nervous system gather sensory information for the central nervous system?
Signup and view all the answers
What occurs during the process of hyperpolarization in a neuron?
Signup and view all the answers
What is the significance of the threshold potential in action potential generation?
Signup and view all the answers
How does the Na/K pump contribute to neuronal activity following an action potential?
Signup and view all the answers
What happens to sodium channels as the membrane potential approaches 40mV during an action potential?
Signup and view all the answers
What defines the excitatory postsynaptic potential (EPSP) in neuronal activity?
Signup and view all the answers
What is the primary function of oxygen in cellular metabolism?
Signup and view all the answers
Which type of transport mechanism utilizes proteins to aid molecule movement across a membrane?
Signup and view all the answers
What are the typical changes observed in coagulative necrosis?
Signup and view all the answers
Which stage of cellular injury involves the cell returning to normal function if stress is relieved early?
Signup and view all the answers
During which process does ATP yield the highest amount of energy in cellular respiration?
Signup and view all the answers
Which of the following best describes secondary active transport?
Signup and view all the answers
What is the consequence of persistent low-level cellular stress?
Signup and view all the answers
Which terminology describes the condition where cellular nuclear material is fragmented?
Signup and view all the answers
What is a characteristic of liquefactive necrosis?
Signup and view all the answers
Which of the following is true regarding the Citric acid/Krebs cycle in terms of ATP production?
Signup and view all the answers
What is the primary function of the Na/K pump in maintaining resting membrane potential?
Signup and view all the answers
Which ion primarily determines the resting membrane potential of a neuron?
Signup and view all the answers
How do K+ leak channels influence the resting membrane potential?
Signup and view all the answers
What does the Nernst Equation calculate for an ion?
Signup and view all the answers
During the process of action potentials, which phase corresponds to the net charge reaching approximately -65mV?
Signup and view all the answers
Which ion's flow into the neuron is primarily responsible for depolarization during an action potential?
Signup and view all the answers
What mechanism allows neurotransmitters to generate action potentials in postsynaptic neurons?
Signup and view all the answers
What effect does the flow of Cl- ions into a neuron generally have?
Signup and view all the answers
What is the primary mechanism through which apoptosis protects an organism from cancer?
Signup and view all the answers
What distinguishes caseous necrosis from liquefactive necrosis?
Signup and view all the answers
Which type of injury is characterized by an increase in intracellular calcium due to ischemia?
Signup and view all the answers
Which of the following is a major consequence of lipid peroxidation?
Signup and view all the answers
During hypoxia, what happens to the pH of the affected tissues?
Signup and view all the answers
Which adaptation involves the increase in cell size without an increase in cell number?
Signup and view all the answers
What type of cellular adaptation occurs in response to chronic injury and is associated with dysregulated cell division?
Signup and view all the answers
Which of the following best describes the process of saponification in fat necrosis?
Signup and view all the answers
Which type of necrosis is often associated with excessive inflammation and results from the revitalization of blood flow in previously ischemic areas?
Signup and view all the answers
Which substance is most commonly associated with causing oxidative stress by producing reactive oxygen species (ROS)?
Signup and view all the answers
What is the relationship between saponification and fat necrosis?
Signup and view all the answers
Which cell injury mechanism is characterized by a decrease in ATP production as a result of mitochondrial swelling?
Signup and view all the answers
What type of response is typically initiated by immune cells that can lead to apoptosis?
Signup and view all the answers
What is a characteristic difference in the chemical messenger used by the nervous system compared to the endocrine system?
Signup and view all the answers
Which statement correctly describes the specificity of action between the nervous and endocrine systems?
Signup and view all the answers
Which of the following correctly identifies the speed of action associated with each system?
Signup and view all the answers
What major function differentiates the roles of the nervous and endocrine systems?
Signup and view all the answers
In terms of anatomical arrangement, how do the nervous and endocrine systems differ?
Signup and view all the answers
What is the primary function of the axon terminal in a neuron?
Signup and view all the answers
Which of the following best describes the role of the autonomic nervous system during stress?
Signup and view all the answers
Which statement correctly differentiates between the types of glial cells involved in myelination?
Signup and view all the answers
In which part of the neuron does the action potential initiate?
Signup and view all the answers
What is a key characteristic of afferent neurons?
Signup and view all the answers
What defines the myelination process carried out by Schwann cells?
Signup and view all the answers
What are the Nodes of Ranvier important for in myelinated neurons?
Signup and view all the answers
Which energy metabolism pathway is unique for requiring oxygen as the final electron acceptor?
Signup and view all the answers
What characterizes facilitated diffusion compared to passive transport?
Signup and view all the answers
Which part of the neuron is primarily responsible for receiving incoming signals?
Signup and view all the answers
What is the expected ATP yield from glycolysis?
Signup and view all the answers
Which mechanism allows for rapid pH regulation in the body?
Signup and view all the answers
Which of the following cellular injuries is indicative of irreversible damage?
Signup and view all the answers
Which type of necrosis results in liquefaction of tissue?
Signup and view all the answers
What characterizes metabolic acidosis?
Signup and view all the answers
How do kidneys contribute to pH balance over time?
Signup and view all the answers
In primary active transport, what underlies the mechanism of moving substances against their concentration gradient?
Signup and view all the answers
Which condition is characterized by an excess loss of non-carbonic acids?
Signup and view all the answers
What best describes chronic cellular stress leading to adaptation?
Signup and view all the answers
Which of the following is NOT a process that cells can undergo due to reversible injury?
Signup and view all the answers
In the event of renal failure, how does the body typically compensate?
Signup and view all the answers
What effect does hyperventilation have on blood chemistry?
Signup and view all the answers
During cellular stress, what is the first observed change in the nucleus typically called?
Signup and view all the answers
What is the primary purpose of active transport mechanisms in cells?
Signup and view all the answers
Which substance forms about 60% of carbon dioxide in the blood?
Signup and view all the answers
What is a likely cause of respiratory acidosis?
Signup and view all the answers
Which buffer system operates both intracellularly and extracellularly?
Signup and view all the answers
What is the primary role of the Na/K pump in maintaining resting membrane potentials?
Signup and view all the answers
Which statement accurately describes the movement of K ions at resting membrane potential?
Signup and view all the answers
What is the equilibrium potential for Na ions based on the provided Nernst equation?
Signup and view all the answers
Which factor primarily influences the establishment of resting membrane potential?
Signup and view all the answers
What initiates the generation of an action potential within a neuron?
Signup and view all the answers
What is the primary significance of the electrostatic gradient in maintaining cellular function?
Signup and view all the answers
Which ion exhibits the greatest movement out of the cell at resting potential and why?
Signup and view all the answers
Which component of the resting membrane potential contributes negatively to the net charge of a neuron?
Signup and view all the answers
What is the significance of reaching the threshold potential of -55mV in neurons?
Signup and view all the answers
Which stage of sodium channels prevents sodium movement during action potential propagation?
Signup and view all the answers
What is primarily responsible for the hyperpolarization of a neuron during an action potential?
Signup and view all the answers
How does the Na/K pump contribute to the action potential process?
Signup and view all the answers
What occurs when the membrane potential reaches 40mV during an action potential?
Signup and view all the answers
Which characteristic of the endocrine system contrasts sharply with that of the nervous system?
Signup and view all the answers
What is the primary function of the nervous system as described?
Signup and view all the answers
Which statement correctly describes the specificity of the endocrine system's chemical messengers?
Signup and view all the answers
What distinguishes the duration of action between the nervous and endocrine systems?
Signup and view all the answers
In what way do the afferent division and endocrine system contribute to sensory processing?
Signup and view all the answers
What effect does an increase in respiratory rate have on the levels of carbon dioxide (CO2) and pH in the blood?
Signup and view all the answers
Which compensation method is employed by the body when metabolic acidosis occurs?
Signup and view all the answers
In respiratory alkalosis, what is the typical state of HCO3- levels?
Signup and view all the answers
What is the primary disturbance observed in respiratory acidosis?
Signup and view all the answers
What distinguishes metabolic alkalosis from metabolic acidosis in terms of bicarbonate levels?
Signup and view all the answers
Which of the following is a cause of metabolic acidosis related to increased acid production?
Signup and view all the answers
Which buffer system operates with both acidic and basic forms in the body?
Signup and view all the answers
In the context of respiratory compensation for acid-base disturbances, what occurs during renal failure?
Signup and view all the answers
What characterizes the metabolic compensation during respiratory alkalosis?
Signup and view all the answers
What is the primary function of the bicarbonate buffer system in the body?
Signup and view all the answers
Which statement accurately describes the ionization of strong and weak acids?
Signup and view all the answers
What does a pH of 7 indicate about a solution?
Signup and view all the answers
Which of the following describes the role of carbonic anhydrase in the bicarbonate buffer system?
Signup and view all the answers
If H+ concentration is low, which direction will the bicarbonate buffer reaction predominantly shift?
Signup and view all the answers
Which of the following best describes how buffer systems function in the body?
Signup and view all the answers
Which arterial blood pH range is considered normal?
Signup and view all the answers
What is the role of the primary buffer systems in the body?
Signup and view all the answers
What type of neuron primarily serves to connect afferent and efferent neurons?
Signup and view all the answers
What is the main function of the nodes of Ranvier in myelinated neurons?
Signup and view all the answers
Which division of the autonomic nervous system is primarily involved in the body's rest and digest functions?
Signup and view all the answers
What is the role of Schwann cells in the peripheral nervous system?
Signup and view all the answers
Which part of a neuron is responsible for synthesizing neurotransmitters?
Signup and view all the answers
What effect does myelination have on action potentials in neurons?
Signup and view all the answers
What is the primary role of the somatic nervous system?
Signup and view all the answers
What characteristic distinguishes afferent neurons from efferent neurons?
Signup and view all the answers
Study Notes
Regulation of CO2 and pH
- Lungs regulate CO2 levels and pH through respiratory rate (RR) changes.
- Increasing RR expels CO2, reducing PCO2 and increasing pH.
- Decreasing RR retains CO2, increasing PCO2 and lowering pH.
- Responses are rapid, occurring within minutes to hours.
- Kidneys manage pH by reabsorbing HCO3- and secreting H+.
- Increased reabsorption and secretion raise pH; decreased reabsorption and secretion lower pH.
- Renal regulation is slower, taking hours to days.
- Approximately 60% of CO2 in blood exists as bicarbonate (HCO3-).
CO2 Transport Forms
- Hemoglobin acts as a buffer, with forms being Hb- (base) and HHb (acid).
- Proteins also buffer pH, existing as Pr- (base) and HPr (acid).
- Phosphate buffering involves HPO4^2- (acid) and H2PO4- (base), present throughout the body including ATP.
Buffer Systems
- Buffer systems function within a specific range to maintain pH levels.
Respiratory and Metabolic Disorders
- Respiratory Acidosis: Low pH, high PCO2, normal HCO3-; caused by hyperventilation and poor gas exchange.
- Respiratory Alkalosis: High pH, low PCO2, normal HCO3-; results from hyperventilation and carbon dioxide depletion.
- Metabolic Acidosis: Low pH, normal PCO2, low HCO3-; due to increased non-carbonic acids (e.g., ketoacidosis, uremia).
- Metabolic Alkalosis: High pH, normal PCO2, high HCO3-; caused by excess loss of non-carbonic acids or bicarbonate intake.
Cell Metabolism and Homeostasis
- Cell metabolism encompasses chemical reactions and energy metabolism for ATP production.
- The nervous and endocrine systems maintain homeostasis through different control mechanisms.
Nervous System Overview
- Central Nervous System (CNS): Comprises the brain and spinal cord.
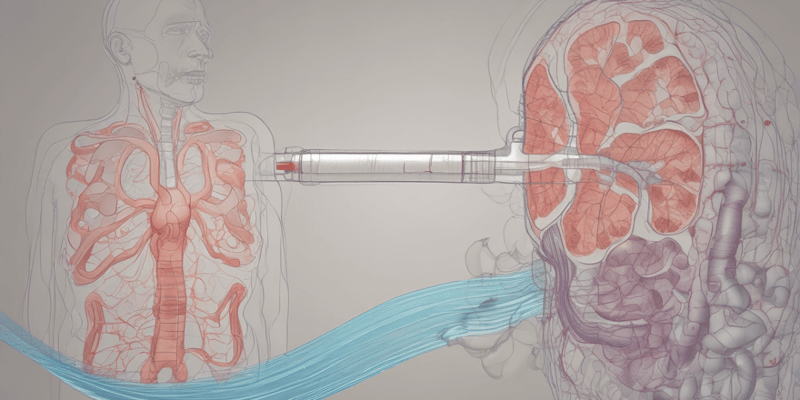
-
Peripheral Nervous System (PNS): Consists of nerves throughout the body, including:
- Afferent Division: Sensory input, linking the body and CNS.
-
Efferent Division: Carries out motor commands, further divided into:
- Somatic Nervous System: Controls voluntary skeletal muscle movement.
-
Autonomic Nervous System: Manages involuntary functions, including:
- Sympathetic Division: Activates fight-or-flight response.
- Parasympathetic Division: Promotes rest and digestion.
Neurons and Signals
- Ramón y Cajal is a key figure in neuroscience, known for developing the Golgi stain for better visualization of neurons.
- Neurons can generate action potentials (APs) through ion movements, crucial for communication.
- Neuron structure includes cell body, dendrites, axon, and terminals, with myelination increasing signal transmission speed.
Action Potentials (AP)
- AP initiation occurs at the axon hillock and propagates along the axon through Na+ channel phases.
- Hyperpolarization follows the depolarization phase, with voltage-gated K+ channels allowing K+ efflux.
- Refractory periods ensure orderly signal propagation, preventing backward movement of APs.
Saltatory Conduction
- In myelinated neurons, APs appear to "jump" between nodes of Ranvier, enhancing conduction efficiency.
Neurotransmitters (NT)
- Classified into amino acids (e.g., glutamate, GABA), monoamines (e.g., acetylcholine, serotonin), and catecholamines (e.g., dopamine).
- Neuroactive peptides influence NT responses, modulating receptor efficacy.
Steps in Chemical Signaling
- Action potential reaches the axon terminal, triggering neurotransmitter release to propagate signals to target cells.
Glycolysis and Cellular Respiration
- Glycolysis takes place in the cytosol, yielding 2 ATP molecules.
- The Citric Acid Cycle (Krebs Cycle) occurs in the mitochondria and also yields 2 ATP.
- Oxidative Phosphorylation, the most ATP-rich step (~32 ATP), occurs in the mitochondria and requires oxygen as the final electron acceptor.
Cell Transport Mechanisms
-
Passive Transport: Movement of molecules without energy.
- Simple diffusion allows molecules like O2 and CO2 to pass freely down their gradient.
- Osmosis refers to water movement toward areas of higher solute concentration.
- Facilitated diffusion uses carrier proteins for molecules like glucose.
-
Active Transport: Requires energy for movement against a gradient.
- Primary active transport directly uses ATP, e.g., Na-K pump.
- Secondary active transport relies on ion gradients created by primary transport.
Cellular Stress and Injury Responses
- Overt injury leads to increased functional demands or reversible injuries that cause adaptations like hypertrophy or atrophy.
- Coagulative necrosis results from external injury, leading to tissue death with characteristic nuclear changes such as pyknosis (nucleus shrinkage) and karyolysis (loss of nucleus).
- Liquefactive necrosis liquefies tissue, seen in areas like the brain.
- Caseous necrosis is a combination of solid and liquefied necrosis, often associated with tuberculosis in lymph nodes.
- Fat necrosis occurs in fatty tissues like the pancreas, resulting in soap-like deposits through saponification.
Apoptosis
- Apoptosis is a programmed cell death mechanism aimed at preventing cancer.
- Key steps include cell activation, shrinkage, nuclear collapse, apoptotic body formation, and lysis of these bodies.
- Triggers include viral infections, DNA damage, and certain stressors.
Mechanisms of Cell Injury
- Hypoxic Injury: Lack of oxygen due to ischemia decreases ATP production and can lead to cell swelling and death.
- Anoxia: Complete oxygen deprivation, often resulting from blood flow blockage.
-
Free Radical Injury: Damage from highly reactive molecules with unpaired electrons, causing lipid peroxidation and DNA damage.
- Common free radicals include superoxide anion and hydroxyl radical.
Cellular Adaptations
- Hypertrophy: Increase in cell size due to greater functional demand; common with weight training.
- Hyperplasia: Increase in cell number without change in size, often occurs with chronic injury.
- Atrophy: Decrease in cell size typically due to decreased demands or hormonal support; e.g., disuse atrophy.
- Metaplasia: Replacement of normal cells with different types, often due to chronic irritation.
- Dysplasia: Increased unregulated cell division; considered precancerous.
Cellular Storage Changes
- Normal cell storage includes fat, glycogen, and water.
- Accumulation can occur due to digestive dysfunction, leading to conditions like fatty liver disease from chronic alcohol use.
Nervous System Control
- Homeostatic control involves sensors, integrators, effectors, and compensatory reactions to maintain set points.
- Divided into somatic (voluntary motor control) and autonomic (involuntary functions).
- Autonomic nervous system includes sympathetic (fight/flight) and parasympathetic (rest/digest) responses.
Nervous Tissue Structure
- Neurons consist of a cell body, dendrites (input), axon hillock (AP initiation), axon (signal transmission), and terminal (neurotransmitter release).
- Myelination enhances AP speed: Schwann cells myelinate PNS neurons; oligodendrocytes myelinate CNS neurons.
- Neuron types include afferent (sensory), interneurons, and efferent (motor) neurons, connecting different nervous system functions.### Nervous System Functioning
- Funx processes afferent signals, generating efferent commands that can target multiple organs.
- Efferent neurons transmit commands from the Central Nervous System (CNS) to target organs, glands, or muscles with cell bodies located in the CNS.
Resting Membrane Potentials
- Dominant ions at rest:
- Intracellular Fluid (ICF): High in potassium (K+) and negatively charged anions.
- Extracellular Fluid (ECF): High in sodium (Na+), chloride (Cl-), and calcium (Ca2+).
- Sodium-Potassium pump actively maintains ion distribution, expelling 3 Na+ ions for every 2 K+ ions taken in.
- Potassium leak channels allow K+ to move out of the cell based on concentration gradients.
- Electrostatic gradients facilitate ion movement to maintain electrical equilibrium.
- Equilibrium potential is determined by both ion concentration gradients and cell permeability to those ions.
- Nernst Equation calculates equilibrium for each ion:
- Single charge ions: ( V = 61.5 \times \log(\frac{[ion]{inside}}{[ion]{outside}}) )
- Double charge ions: ( V = 30.75 \times \log(\frac{[ion]{inside}}{[ion]{outside}}) )
- Specific equilibrium values:
- Potassium (K+): approximately -92 mV
- Calcium (Ca2+): approximately 123 mV
- Sodium (Na+): approximately 67 mV
- Chloride (Cl-): approximately -86 mV
- Ion movement during resting potential:
- K+: primarily moves out, significant flow (90%)
- Ca2+: minimal movement in (1%)
- Na+: minimal movement in (1%)
- Cl-: modest movement in (8%)
Action Potentials (AP)
- AP represents an electrical signal generated within a neuron.
- Neurotransmitters (NT) bind to dendrites, opening ion channels and initiating AP at the axon hillock.
- Net charge of a neuron at rest is about -65 mV.
- Steps in generating an action potential:
- NT binding leads to depolarization.
- Refractory periods:
- Absolute refractory period: Na+ channels are inactive, preventing backflow or close consecutive APs.
- Relative refractory period: Na+ channels closed; a stronger stimulus required to generate an AP due to hyperpolarization (around -75 mV).
- Saltatory conduction occurs in myelinated neurons, where Na+ ions effectively "bump" into neighboring Na+ ions within the myelin sheath, creating the appearance of the AP jumping between nodes of Ranvier.
Interneural Communication
- Neurons communicate either electrically or chemically via synapses.
- Chemical communication involves excitatory or inhibitory neurotransmitters released by presynaptic cells and received by postsynaptic cells.
Neurotransmitters
- Key categories of neurotransmitters include:
-
Amino Acids:
- Glutamic Acid (glutamate): stimulatory, prevalent throughout the CNS.
- Aminobutyric Acid (GABA): primary inhibitory neurotransmitter.
- Glycine: another generic inhibitory neurotransmitter.
- Monoamines: modified amino acids such as acetylcholine and serotonin.
- Catecholamines: derived from tyrosine, include dopamine, norepinephrine (NE), and epinephrine.
-
Amino Acids:
- Neuroactive peptides: peptide molecules that modulate neurotransmitter effects without acting solely as neurotransmitters; often enhance receptor response in postsynaptic cells e.g. endorphins, substance P, neurotensin, and others.
Steps of Chemical Messaging
- AP travels to the axon terminal, prompting neurotransmitter release and subsequent signal transmission to the next neuron.
Glycolysis and Energy Metabolism
- Glycolysis occurs in the cytosol of cells, yielding 2 ATP.
- The Citric Acid (Krebs) Cycle takes place in the mitochondria and also yields 2 ATP.
- Oxidative Phosphorylation, located in the mitochondria, produces approximately 32 ATP, making it the largest contributor to ATP yield.
- Oxygen is essential in oxidative phosphorylation as the final electron acceptor.
Cell Transport Mechanisms
- Passive transport involves the movement of molecules without energy, including:
- Simple diffusion: molecules move across the membrane down their gradient (e.g., O2, CO2).
- Osmosis: water movement towards areas of high solute concentration (e.g., water follows Na).
- Facilitated diffusion: requires carrier proteins or protein channels (e.g., glucose).
- Active transport requires energy for movement:
- Secondary active transport uses ATP to move molecules against their gradient (e.g., Na-K pump).
- Primary active transport relies on the electrochemical gradient established by primary transport (e.g., Na-glucose cotransporter).
Cellular Stress and Injury
- Stress or overt injury leads to increased functional demand or reversible cell injury.
- Adaptations to persistent stress include hypertrophy (cell enlargement) and hyperplasia (increased cell number).
- Coagulative necrosis refers to cell death from external causes, resulting in generalized tissue death with significant cellular changes.
- Different types of necrosis include:
- Liquefactive necrosis: forming a liquid mass due to cell death in areas with little connective tissue.
- Caseous necrosis: partially liquefied tissue resembling cottage cheese, commonly seen in TB-infected lymph nodes.
- Fat necrosis: occurs in fatty tissues (e.g., pancreas) and involves saponification.
Apoptosis
- Apoptosis is a programmed cell death designed to protect organisms from potential cancerous cells.
- Key steps in apoptosis:
- Activation, cell shrinkage, chromatin condensation, nuclear collapse, and formation of apoptotic bodies.
- Triggers include viral infection, DNA damage, mitochondrial damage, and cell stress.
Mechanisms of Cell Injury
- Hypoxic injury arises from insufficient oxygen supply, leading to bioenergetic failure and cell death.
- Anoxia is complete loss of oxygen delivery commonly due to blood flow blockage.
- Free radical injury involves reactive oxygen species harming cells, leading to lipid peroxidation, protein damage, and DNA damage.
- Common free radicals include superoxide anions, peroxides, and hydroxyl radicals.
- Cellular adaptations to injury may include hypertrophy, hyperplasia, atrophy, metaplasia, and dysplasia; signaling pathways differ.
Adaptations to Stress
- Hypertrophy increases cell size without increasing cell number, stemming from heightened functional demands or hormonal stimulation.
- Hyperplasia results in increased cell numbers, often accompanying hypertrophy.
- Atrophy is characterized by decreased cell size while maintaining cell numbers, often due to diminished functional demand or hormonal levels.
- Metaplasia involves the transformation of one type of cell into another more resilient type in response to chronic injury.
- Dysplasia refers to abnormal cell division, pre-cancerous in nature, particularly affecting epithelial tissues.
Changes in Cell Storage
- Normal cellular storage involves lipids, glycogen, and vesicles of water.
- Accumulation may occur from enzyme deficiencies, as seen in Tay-Sachs disease or fatty liver disease related to chronic ethanol exposure.
- Hydropic swelling involves expansion of organelles due to injurious stimuli like hypoxia.
Nervous System Functionality
- Homeostatic control systems manage deviations from set points using sensors, integrators, effectors, and compensatory reactions.
- The nervous system operates via a wired network with rapid responses and brief actions through neurotransmitters.
- The endocrine system functions via a wireless network, employing hormones for long-distance signaling, slow reactions, with lasting effects.
Nervous System Divisions
- Central Nervous System (CNS): comprises the brain and spinal cord.
- Peripheral Nervous System (PNS): encompasses nerves throughout the body.
- Afferent division of PNS receives sensory information including touch, heat, and pain signals.### Neurons and Signaling
- Funx processes afferent signals to generate efferent commands, targeting multiple organs or muscles.
- Efferent neurons transmit commands from the central nervous system (CNS) to target organs, glands, or muscles.
- Cell body of efferent neurons is located in the CNS.
Resting Membrane Potentials
- Dominant ions at rest:
- Intracellular Fluid (ICF): Potassium (K+), negatively charged ions (A-).
- Extracellular Fluid (ECF): Sodium (Na+), Chloride (Cl-), Calcium (Ca2+).
- Na+/K+ pump maintains ion distributions by moving 3 Na+ ions out and 2 K+ ions in.
- K+ leak channels allow potassium ions to move freely out based on concentration gradients.
- Electrostatic gradient facilitates ion movement to maintain electrical equilibrium.
- Equilibrium potential is influenced by concentration gradients and membrane permeability to ions.
- Nernst Equation calculates equilibrium for single and double charged ions, providing specific equilibrium potentials:
- K+: -92 mV
- Ca2+: -123 mV
- Na+: +67 mV
- Cl-: -86 mV (negative charge due to internal conditions).
- Ion movement specifics:
- K+ predominantly moves out, leading to a negative potential.
- Ca2+ and Na+ have minimal inward movement.
- Cl- moves in, adjusting overall charge.
Action Potentials (AP)
- Action potentials are electrical signals generated within neurons.
- Neurotransmitters (NTs) bind to dendrites, opening ion channels to create APs at the axon hillock.
- Initial net charge of the cell at rest is approximately -65 mV.
- Steps of an action potential:
- NT binding to ligand triggers Na+ channel opening, leading to cell depolarization.
- Excitatory postsynaptic potential (EPSP) increases cell positivity; inhibitory postsynaptic potential (IPSP) enhances negativity through Cl- channels.
- Threshold potential of -55 mV is required to initiate an AP.
- AP propagates along the axon as Na+ channels sequentially open, reaching a peak of 40 mV.
- Stages of Na+ channel status:
- Closed: no Na+ flow.
- Open: free Na+ movement.
- Inactivated: blocked and prevents Na+ movement, aiding repolarization.
- Stages of Na+ channel status:
- After peak, hyperpolarization occurs, dropping the charge to -75 mV as K+ channels open at 40 mV.
- This response is slower and contributes to hyperpolarization.
- The Na+/K+ pump operates continuously to assist in repolarizing the membrane and stabilizing resting potential.
Respiratory Regulation of CO2
- Lungs regulate CO2 through respiratory rate (RR) and depth.
- Increased RR eliminates CO2, decreasing PCO2 and pH.
- Decreased RR preserves CO2, increasing PCO2 and decreasing pH.
- Response time: Minutes to hours.
Renal Regulation of pH
- Kidneys regulate pH by reabsorbing HCO3- and secreting H+.
- Increased HCO3- reabsorption and H+ secretion raise pH.
- Decreased HCO3- reabsorption lowers pH.
- Response time: Hours to days.
Carbon Dioxide Transport in Blood
- 60% of CO2 is transported as bicarbonate (HCO3-) in the blood.
- Hemoglobin exists as deoxygenated (HHb) and oxygenated (Hb) forms.
- Proteins in the blood also contribute to acid-base balance.
Buffer Systems
- Buffer systems operate within a specific pH range, enhancing pH maintenance.
Acid-Base Disorders
-
Respiratory Acidosis
- Low pH, high PCO2, normal HCO3-.
- Causes: Hyperventilation, poor gas exchange; CO2 accumulation.
-
Respiratory Alkalosis
- High pH, low PCO2, normal HCO3-.
- Causes: Hyperventilation; CO2 depletion.
-
Metabolic Acidosis
- Low pH, normal PCO2, low HCO3-.
- Causes: Increased non-carbonic acids (ketoacidosis, uremia) and bicarbonate loss (diarrhea).
-
Metabolic Alkalosis
- High pH, normal PCO2, high HCO3-.
- Causes: Excess loss of non-carbonic acids (vomiting) or bicarbonate intake.
Cell Metabolism
- Involves chemical reactions for energy (ATP) production.
-
Metabolic Steps:
- Glycolysis: 2 ATP yield, occurs in cytosol.
- Krebs Cycle: 2 ATP yield, occurs in mitochondria.
- Oxidative Phosphorylation: ~32 ATP yield, requires oxygen.
Cell Transport Mechanisms
-
Passive Transport: No energy required.
- Simple diffusion (e.g., O2, CO2).
- Osmosis (e.g., water movement).
- Facilitated diffusion (e.g., glucose with protein channels).
-
Active Transport: Energy required.
- Secondary active transport (e.g., Na-K pump).
- Primary active transport (e.g., Na-glucose cotransporter).
Cellular Stress and Injury
- Stress leads to functional demand increases or injury.
- Can result in adaptations like hypertrophy or reversible injury changes (atrophy or dysplasia).
- Severe injury can lead to coagulative necrosis (cell death).
- Coagulative Necrosis: General tissue death, characterized by coagulation of proteins and cell components.
- Liquefactive Necrosis: Tissue liquefies due to lack of connective tissue; common in endocrine systems.
Nervous System Functions
-
Control Systems: Regulate homeostasis.
-
Nervous System Characteristics:
- Wired system with rapid, short-distance signal transmission via neurotransmitters.
-
Endocrine System Characteristics:
- Wireless system utilizing hormones for long-distance action, with slower response times.
Nervous Tissue Structure
- Neurons are the primary cells; their structure includes:
- Cell body (soma).
- Dendrites receive signals.
- Axon and axon terminals transmit signals.
- Myelination enhances signal flow.
Resting Membrane Potential
- Dominant ions differ between intracellular (K+, A-) and extracellular (Na+, Cl-, Ca2+) environments.
- Na/K Pump: Transports 3 Na+ out and 2 K+ in, maintaining ion balance.
- K leak channels allow passive K+ movement, affecting electrical equilibrium.
Action Potentials (AP)
- AP is an electrical signal initiated when neurotransmitters bind to dendrites, opening ion channels.
- Net charge of the resting cell is approximately -65mV.
Key Equations for Membrane Potentials
- Nernst Equation used for calculating equilibrium potentials.
- Membrane potential influenced by ion concentrations and permeability.
These notes capture key concepts and information regarding respiratory and renal regulation, cellular metabolism and transport, nervous system functions, and the mechanisms of cell injury and membrane potentials.
Acid-Base Balance
- Acids donate H+ ions to solutions; strong acids fully ionize while weak acids partially ionize (e.g., acetic acid).
- Bases absorb H+ ions; acetate acts as a weak base by absorbing H+ to form acetic acid.
- pH measures H+ concentration, calculated as pH = -log[H+]; normal arterial blood pH ranges from 7.38 to 7.42.
- Buffers are weak acids/bases that maintain pH in body fluids, with kidneys and lungs as primary regulators.
- Major buffer systems include bicarbonate (HCO3- as base and H2CO3 as acid), hemoglobin (Hb- and HHb), proteins (Pr- and HPr), and phosphate (H2PO4- and HPO4=).
- Compensatory responses exist for pH imbalances to stabilize blood pH.
Respiratory and Metabolic Disorders
- Respiratory Acidosis: Characterized by low pH and high PCO2; caused by hyperventilation or poor gas exchange. Compensation occurs through renal adjustments.
- Respiratory Alkalosis: High pH and low PCO2 levels; results from hyperventilation and CO2 depletion, requiring renal compensation.
- Metabolic Acidosis: Low pH with normal PCO2 and low HCO3-; may result from ketoacidosis, uremia, or diarrhea leading to bicarbonate loss.
- Metabolic Alkalosis: High pH, normal PCO2, and elevated HCO3-; causes include prolonged vomiting and hyperaldosteronism.
Cell Metabolism
- Cell metabolism involves various chemical reactions for energy (ATP) production.
- Energy metabolism specifically focuses on nutrient breakdown to generate ATP.
Nervous System Overview
- Central Nervous System (CNS): Comprises the brain and spinal cord.
- Peripheral Nervous System (PNS): Includes all nerves outside the CNS, divided into afferent (sensory) and efferent (motor) divisions.
- Afferent division receives sensory information (e.g., temperature, pain, blood pressure).
- Efferent division executes motor commands, with somatic (voluntary) and autonomic (involuntary) subtypes.
- Autonomic nervous system consists of sympathetic (fight/flight response) and parasympathetic (rest/digest) pathways.
Nervous Tissue Structures
- Ramón y Cajal, a key figure in neuroscience, developed the Golgi stain to visualize neurons.
- Neurons are the primary cells in the nervous system, characterized by their ability to generate action potentials (AP).
- Neuron structure includes:
- Soma: contains organelles and neurotransmitter vesicles.
- Dendrites: receive input from other neurons.
- Axon: transmits electrical impulses.
- Myelination increases AP speed and preserves signal integrity; Schwann cells myelinate PNS neurons, whereas oligodendrocytes myelinate CNS neurons.
Neuron Types and Functioning
- Afferent Neurons: Carry sensory information to the CNS, with cell bodies located in the PNS.
- Interneurons: Connect afferent and efferent neurons, facilitating signal transmission.
- Action potentials are triggered when the membrane reaches threshold potential (-55mV), involving the opening and closing of sodium channels.
- Hyperpolarization occurs when the membrane potential drops below resting levels due to potassium movement, while sodium/potassium pumps restore balance.
Key Concepts in Action Potential
- Succession of Na channel states (closed, open, inactivated) regulates the AP mechanisms.
- The rapid reactions of the nervous system are critical for precise control and response to stimuli, while the endocrine system facilitates broader regulatory functions through hormonal signaling.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Related Documents
Description
This quiz covers the vital role of the lungs in regulating respiratory rate (RR) and depth. It explores how changes in RR can affect carbon dioxide (CO2) levels and, consequently, blood pH. Understanding these mechanisms is crucial for grasping respiratory physiology.