Podcast
Questions and Answers
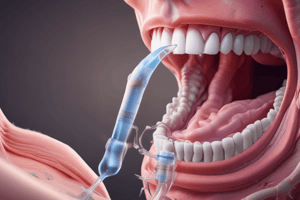
Which of the following statements are true regarding oropharyngeal airways (OPAs)?
Which of the following statements are true regarding oropharyngeal airways (OPAs)?
- OPAs should not be used during bag-mask ventilation. (correct)
- An OPA should be used in patients with an intact gag reflex.
- An OPA may be inserted in cases requiring repeated suctioning.
- To measure an OPA, note the distance from the corner of the mouth to the earlobe.
For a patient requiring mechanical ventilation, which of the following blood gas values most strongly indicates the need for intervention?
For a patient requiring mechanical ventilation, which of the following blood gas values most strongly indicates the need for intervention?
- pH of 7.30
- pH of 7.40
- pH of 7.35
- pH of 7.26 (correct)
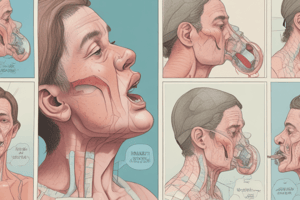
A 60-year-old female patient who is 5'8" and weighs 88 kg requires intubation. Which size laryngoscope blade, endotracheal tube (ETT) size, and technique would be most appropriate?
A 60-year-old female patient who is 5'8" and weighs 88 kg requires intubation. Which size laryngoscope blade, endotracheal tube (ETT) size, and technique would be most appropriate?
- Mac 3.0, ETT 4.0, and lift the epiglottis to place the ETT.
- Miller 7.0, ETT 3.0, and lift either the epiglottis or vallecula to place the ETT.
- Miller 4.0, ETT 9.0, and lift the epiglottis to place the ETT.
- Mac 3.0, ETT 7.0, and place the blade in the vallecula. (correct)
During mechanical ventilation, you notice a leak around the endotracheal tube of a 35-year-old female patient with a 6.5 ETT. What is the most appropriate initial action to resolve the leak?
During mechanical ventilation, you notice a leak around the endotracheal tube of a 35-year-old female patient with a 6.5 ETT. What is the most appropriate initial action to resolve the leak?
Which statement is false regarding Minimal Leak Technique (MLT) and Minimal Occlusion Volume (MOV)?
Which statement is false regarding Minimal Leak Technique (MLT) and Minimal Occlusion Volume (MOV)?
You want to increase the volume delivered to a patient in pressure control (PC) mode. Which actions will help?
You want to increase the volume delivered to a patient in pressure control (PC) mode. Which actions will help?
If the goal is to keep the delivered volume constant while increasing the flow on a mechanical ventilator, what adjustment should be made to the inspiratory time?
If the goal is to keep the delivered volume constant while increasing the flow on a mechanical ventilator, what adjustment should be made to the inspiratory time?
Which of the following statements are true regarding ventilation?
Which of the following statements are true regarding ventilation?
A physician orders a high tidal volume ($12 \text{ml/kg}$) for a patient on mechanical ventilation. What is the most appropriate action to prevent potential lung injury?
A physician orders a high tidal volume ($12 \text{ml/kg}$) for a patient on mechanical ventilation. What is the most appropriate action to prevent potential lung injury?
Which of the following statements is true regarding PEEP (Positive End-Expiratory Pressure)?
Which of the following statements is true regarding PEEP (Positive End-Expiratory Pressure)?
A physician asks you to initiate mechanical ventilation on a female patient, 6'1" tall and weighing 88 kg, who has overdosed on drugs. Which settings for tidal volume (Vt), rate (f), and mode would be most appropriate?
A physician asks you to initiate mechanical ventilation on a female patient, 6'1" tall and weighing 88 kg, who has overdosed on drugs. Which settings for tidal volume (Vt), rate (f), and mode would be most appropriate?
Which of the following statements is true regarding pressure support ventilation (PSV)?
Which of the following statements is true regarding pressure support ventilation (PSV)?
A patient presents with the following ABGs while having increased WOB: pH 7.47, PaCO2 32, PaO2 48, HCO3 25. Their condition is likely related to fluid overload. What is the most appropriate respiratory intervention?
A patient presents with the following ABGs while having increased WOB: pH 7.47, PaCO2 32, PaO2 48, HCO3 25. Their condition is likely related to fluid overload. What is the most appropriate respiratory intervention?
If the inspiratory time (I-time) is increased while the flow remains constant, what effect will this have on the tidal volume (Vt)?
If the inspiratory time (I-time) is increased while the flow remains constant, what effect will this have on the tidal volume (Vt)?
A patient is on the ventilator in A/C, with these settings: Vt 400, f 14, PEEP 5, and FiO2 0.50. Post-intubation ABGs show: pH 7.30, PaCO2 74, and PaO2 62. Pre-intubation ABGs showed pH 7.24, PaCO2 82, and PaO2 48. The physician wants a compensated pH with a PaCO2 of 40 torr and allows increasing Vt up to 500. What is most appropriate?
A patient is on the ventilator in A/C, with these settings: Vt 400, f 14, PEEP 5, and FiO2 0.50. Post-intubation ABGs show: pH 7.30, PaCO2 74, and PaO2 62. Pre-intubation ABGs showed pH 7.24, PaCO2 82, and PaO2 48. The physician wants a compensated pH with a PaCO2 of 40 torr and allows increasing Vt up to 500. What is most appropriate?
Which of the following best describes the correct insertion technique for a nasopharyngeal airway (NPA)?
Which of the following best describes the correct insertion technique for a nasopharyngeal airway (NPA)?
What is the primary indication for using an oropharyngeal airway (OPA)?
What is the primary indication for using an oropharyngeal airway (OPA)?
A patient with a pH of 7.20 is likely experiencing which of the following?
A patient with a pH of 7.20 is likely experiencing which of the following?
Which of the following is the most appropriate initial cuff pressure for a Laryngeal Mask Airway (LMA)?
Which of the following is the most appropriate initial cuff pressure for a Laryngeal Mask Airway (LMA)?
Which of the following scenarios represents a prophylactic indication for mechanical ventilation?
Which of the following scenarios represents a prophylactic indication for mechanical ventilation?
What is the primary risk associated with high tidal volumes during mechanical ventilation?
What is the primary risk associated with high tidal volumes during mechanical ventilation?
Which of the following is a key consideration when selecting the appropriate size endotracheal tube (ETT) for adult patients?
Which of the following is a key consideration when selecting the appropriate size endotracheal tube (ETT) for adult patients?
What is the primary purpose of the pressure limit setting on a mechanical ventilator?
What is the primary purpose of the pressure limit setting on a mechanical ventilator?
After initiating mechanical ventilation, a patient's PaCO2 increases significantly. What ventilator adjustment would be most effective in lowering the PaCO2?
After initiating mechanical ventilation, a patient's PaCO2 increases significantly. What ventilator adjustment would be most effective in lowering the PaCO2?
What does the formula $V_E = Vt \times f$ represent?
What does the formula $V_E = Vt \times f$ represent?
A patient on mechanical ventilation has a Total Cycle Time (TCT) of 4 seconds and an I:E ratio of 1:3. What is the inspiratory time (I-time)?
A patient on mechanical ventilation has a Total Cycle Time (TCT) of 4 seconds and an I:E ratio of 1:3. What is the inspiratory time (I-time)?
The physician asks you to administer mechanical ventilation on a patient in respiratory failure and states that they prefer Volume Control. Determine which of the following settings are most crucial to set, versus which parameters the ventilator can adjust automatically.
The physician asks you to administer mechanical ventilation on a patient in respiratory failure and states that they prefer Volume Control. Determine which of the following settings are most crucial to set, versus which parameters the ventilator can adjust automatically.
A mechanically ventilated patient has developed ARDS. The physician wants to use an inverse I:E ratio to improve oxygenation. Which I:E ratio would be most appropriate in this situation?
A mechanically ventilated patient has developed ARDS. The physician wants to use an inverse I:E ratio to improve oxygenation. Which I:E ratio would be most appropriate in this situation?
In the context of ventilator graphics, what does a 'loop' typically represent?
In the context of ventilator graphics, what does a 'loop' typically represent?
A patient is on Assist Control. The patient's spontaneous respiratory effort triggers a ventilator breath, but the breath is delivered before they can begin an active breath. The physician asks you to adjust the sensitivity to ensure patient ventilator synchrony. Considering the parameters of sensitivity, what is the correct action?
A patient is on Assist Control. The patient's spontaneous respiratory effort triggers a ventilator breath, but the breath is delivered before they can begin an active breath. The physician asks you to adjust the sensitivity to ensure patient ventilator synchrony. Considering the parameters of sensitivity, what is the correct action?
Upon insertion of an oropharyngeal airway (OPA) in an adult patient, you note the patient begins to gag and shows signs of regaining consciousness. What is the MOST appropriate immediate action?
Upon insertion of an oropharyngeal airway (OPA) in an adult patient, you note the patient begins to gag and shows signs of regaining consciousness. What is the MOST appropriate immediate action?
A patient with a known history of nasal trauma and a deviated septum requires airway management. Which airway adjunct is MOST appropriate?
A patient with a known history of nasal trauma and a deviated septum requires airway management. Which airway adjunct is MOST appropriate?
In a patient with a confirmed pneumothorax requiring mechanical ventilation, which ventilator strategy is MOST crucial to minimize further lung injury?
In a patient with a confirmed pneumothorax requiring mechanical ventilation, which ventilator strategy is MOST crucial to minimize further lung injury?
A 70 kg ARDS patient is being mechanically ventilated. The physician requests you maintain a plateau pressure close to $30 ext{cmH2O}$. Which combination of settings is MOST likely to achieve this goal?
A 70 kg ARDS patient is being mechanically ventilated. The physician requests you maintain a plateau pressure close to $30 ext{cmH2O}$. Which combination of settings is MOST likely to achieve this goal?
A patient on mechanical ventilation suddenly exhibits increased airway pressures, audible wheezing, and decreased breath sounds on the left side. What is the MOST likely cause?
A patient on mechanical ventilation suddenly exhibits increased airway pressures, audible wheezing, and decreased breath sounds on the left side. What is the MOST likely cause?
A physician orders mechanical ventilation for a patient with severe COPD exacerbation. Which ventilator strategy is MOST appropriate to minimize the risk of air trapping and alveolar overdistension?
A physician orders mechanical ventilation for a patient with severe COPD exacerbation. Which ventilator strategy is MOST appropriate to minimize the risk of air trapping and alveolar overdistension?
A patient on pressure support ventilation (PSV) exhibits signs of increasing respiratory fatigue, including tachypnea and increased accessory muscle use. Which ventilator adjustment is MOST appropriate to reduce their work of breathing?
A patient on pressure support ventilation (PSV) exhibits signs of increasing respiratory fatigue, including tachypnea and increased accessory muscle use. Which ventilator adjustment is MOST appropriate to reduce their work of breathing?
A patient with ARDS is being ventilated with high PEEP. Following a PEEP increase, blood pressure drops significantly. What is the MOST likely cause?
A patient with ARDS is being ventilated with high PEEP. Following a PEEP increase, blood pressure drops significantly. What is the MOST likely cause?
Which of the following BEST describes the rationale for using an inspiratory pause (plateau pressure check) during mechanical ventilation?
Which of the following BEST describes the rationale for using an inspiratory pause (plateau pressure check) during mechanical ventilation?
A patient on mechanical ventilation develops metabolic acidosis. How will the ventilator respond if set in PRVC (Pressure Regulated Volume Control)?
A patient on mechanical ventilation develops metabolic acidosis. How will the ventilator respond if set in PRVC (Pressure Regulated Volume Control)?
After intubating a patient, the capnography reading is unexpectedly low (near zero). Auscultation reveals breath sounds are present only on the right side of the chest. What is the MOST appropriate next step?
After intubating a patient, the capnography reading is unexpectedly low (near zero). Auscultation reveals breath sounds are present only on the right side of the chest. What is the MOST appropriate next step?
A patient is being mechanically ventilated in Assist Control (A/C) mode. They begin to trigger the ventilator at a much higher rate than the set rate, leading to respiratory alkalosis. What adjustment is MOST appropriate?
A patient is being mechanically ventilated in Assist Control (A/C) mode. They begin to trigger the ventilator at a much higher rate than the set rate, leading to respiratory alkalosis. What adjustment is MOST appropriate?
Which of the following BEST describes the primary goal of permissive hypercapnia in mechanically ventilated patients with Acute Respiratory Distress Syndrome (ARDS)?
Which of the following BEST describes the primary goal of permissive hypercapnia in mechanically ventilated patients with Acute Respiratory Distress Syndrome (ARDS)?
A patient with a traumatic brain injury is mechanically ventilated. The physician wants to maintain a PaCO2 between 30-35 mmHg. Which ventilator adjustment is MOST appropriate to achieve this?
A patient with a traumatic brain injury is mechanically ventilated. The physician wants to maintain a PaCO2 between 30-35 mmHg. Which ventilator adjustment is MOST appropriate to achieve this?
A patient on mechanical ventilation suddenly develops severe agitation and starts "fighting" the ventilator. Initial assessment reveals normal vital signs and no obvious signs of distress. What should you do?
A patient on mechanical ventilation suddenly develops severe agitation and starts "fighting" the ventilator. Initial assessment reveals normal vital signs and no obvious signs of distress. What should you do?
Given the complexities of airway management, which of the following statements regarding the clinical application of oropharyngeal (OPA) and nasopharyngeal (NPA) airways is MOST accurate in a patient with maxillofacial trauma and suspected basilar skull fracture?
Given the complexities of airway management, which of the following statements regarding the clinical application of oropharyngeal (OPA) and nasopharyngeal (NPA) airways is MOST accurate in a patient with maxillofacial trauma and suspected basilar skull fracture?
Considering the intricacies of Laryngeal Mask Airway (LMA) usage during prolonged mechanical ventilation, which of the following statements represents the MOST critical consideration for ensuring patient safety and minimizing complications?
Considering the intricacies of Laryngeal Mask Airway (LMA) usage during prolonged mechanical ventilation, which of the following statements represents the MOST critical consideration for ensuring patient safety and minimizing complications?
Given the complexities of mechanical ventilation, which of the following scenarios represents the MOST nuanced indication for prophylactic mechanical ventilation in a patient with rapidly progressing Guillain-Barré syndrome?
Given the complexities of mechanical ventilation, which of the following scenarios represents the MOST nuanced indication for prophylactic mechanical ventilation in a patient with rapidly progressing Guillain-Barré syndrome?
In the context of endotracheal tube (ETT) selection for a neonate with Pierre Robin sequence and micrognathia undergoing surgical correction of a cleft palate, which of the following considerations is MOST critical for ensuring appropriate tube fit and minimizing complications?
In the context of endotracheal tube (ETT) selection for a neonate with Pierre Robin sequence and micrognathia undergoing surgical correction of a cleft palate, which of the following considerations is MOST critical for ensuring appropriate tube fit and minimizing complications?
Considering the complexities of ventilator management, which of the following refinements to ventilator settings is MOST appropriate immediately after intubation to mitigate further lung injury?
Considering the complexities of ventilator management, which of the following refinements to ventilator settings is MOST appropriate immediately after intubation to mitigate further lung injury?
What fundamental principle underlies the calculation of minute ventilation ($V_E = Vt imes f$) and its direct influence on arterial carbon dioxide tension ($PaCO_2$)?
What fundamental principle underlies the calculation of minute ventilation ($V_E = Vt imes f$) and its direct influence on arterial carbon dioxide tension ($PaCO_2$)?
For a patient on mechanical ventilation with a Total Cycle Time (TCT) of 4 seconds and an I:E ratio of 1:3, which of the following BEST explains the physiological implication of this inspiratory time (I-time) on gas exchange and ventilator management?
For a patient on mechanical ventilation with a Total Cycle Time (TCT) of 4 seconds and an I:E ratio of 1:3, which of the following BEST explains the physiological implication of this inspiratory time (I-time) on gas exchange and ventilator management?
In managing a patient with severe Acute Respiratory Distress Syndrome (ARDS) on mechanical ventilation, which strategy reflects the MOST comprehensive integration of lung-protective ventilation principles when implementing an inverse I:E ratio?
In managing a patient with severe Acute Respiratory Distress Syndrome (ARDS) on mechanical ventilation, which strategy reflects the MOST comprehensive integration of lung-protective ventilation principles when implementing an inverse I:E ratio?
Given the intricacies of interpreting ventilator graphics, what is the MOST clinically relevant interpretation of a "beak" appearing at the end of the inspiratory phase of a pressure-volume loop?
Given the intricacies of interpreting ventilator graphics, what is the MOST clinically relevant interpretation of a "beak" appearing at the end of the inspiratory phase of a pressure-volume loop?
In the context of mechanical ventilation in Assist Control (A/C) mode, what is the MOST precise and nuanced adjustment of ventilator sensitivity required to ensure optimal patient-ventilator synchrony?
In the context of mechanical ventilation in Assist Control (A/C) mode, what is the MOST precise and nuanced adjustment of ventilator sensitivity required to ensure optimal patient-ventilator synchrony?
In a patient being mechanically ventilated for severe traumatic brain injury (TBI), the physician aims to maintain a PaCO2 between 30-35 mmHg. To achieve this specific PaCO2 target WHILE simultaneously minimizing the risk of secondary brain injury, which ventilator adjustment should be MOST carefully considered and implemented?
In a patient being mechanically ventilated for severe traumatic brain injury (TBI), the physician aims to maintain a PaCO2 between 30-35 mmHg. To achieve this specific PaCO2 target WHILE simultaneously minimizing the risk of secondary brain injury, which ventilator adjustment should be MOST carefully considered and implemented?
In a patient on mechanical ventilation who begins actively "fighting" the ventilator despite normal vital signs and no obvious signs of distress, which of the following is the MOST judicious and nuanced approach to addressing this acute agitation?
In a patient on mechanical ventilation who begins actively "fighting" the ventilator despite normal vital signs and no obvious signs of distress, which of the following is the MOST judicious and nuanced approach to addressing this acute agitation?
Considering the complex interplay of ventilator parameters in a patient with COPD exacerbation, which ventilator strategy is MOST likely to minimize the risk of air trapping and alveolar overdistension?
Considering the complex interplay of ventilator parameters in a patient with COPD exacerbation, which ventilator strategy is MOST likely to minimize the risk of air trapping and alveolar overdistension?
Which of the following statements MOST accurately reflects the nuanced approach towards ventilator circuit changes?
Which of the following statements MOST accurately reflects the nuanced approach towards ventilator circuit changes?
In a female patient, 5'4" (162 cm) and weighing 68 kg, requiring prophylactic intubation, which initial ventilator settings should be most precisely considered immediately following administration of a paralytic to optimize lung mechanics and minimize potential harm?
In a female patient, 5'4" (162 cm) and weighing 68 kg, requiring prophylactic intubation, which initial ventilator settings should be most precisely considered immediately following administration of a paralytic to optimize lung mechanics and minimize potential harm?
Flashcards
OPAs and NPAs
OPAs and NPAs
Artificial airways used to maintain upper airway patency.
Oropharyngeal Airway (OPA)
Oropharyngeal Airway (OPA)
Used for unconscious patients to prevent tongue obstruction.
Nasopharyngeal Airway (NPA)
Nasopharyngeal Airway (NPA)
Inserted into the nostril to maintain airway patency, even in conscious patients.
Laryngeal Mask Airway (LMA)
Laryngeal Mask Airway (LMA)
Signup and view all the flashcards
Mechanical Ventilation (MV) objective
Mechanical Ventilation (MV) objective
Signup and view all the flashcards
Primary Objectives of MV
Primary Objectives of MV
Signup and view all the flashcards
Main Settings of MV
Main Settings of MV
Signup and view all the flashcards
Heated humidifiers
Heated humidifiers
Signup and view all the flashcards
Increase volume in PC mode
Increase volume in PC mode
Signup and view all the flashcards
Barotrauma
Barotrauma
Signup and view all the flashcards
Volutrauma
Volutrauma
Signup and view all the flashcards
Two Main Categories of MV
Two Main Categories of MV
Signup and view all the flashcards
PEEP
PEEP
Signup and view all the flashcards
P/F Ratio Definition
P/F Ratio Definition
Signup and view all the flashcards
Total Cycle Time (TCT)
Total Cycle Time (TCT)
Signup and view all the flashcards
OPA Use
OPA Use
Signup and view all the flashcards
NPA Insertion
NPA Insertion
Signup and view all the flashcards
Measuring an OPA
Measuring an OPA
Signup and view all the flashcards
Airway devices in bag mask ventilation
Airway devices in bag mask ventilation
Signup and view all the flashcards
Indications for MV
Indications for MV
Signup and view all the flashcards
Indications for artificial airway and mechanical ventilation?
Indications for artificial airway and mechanical ventilation?
Signup and view all the flashcards
Intubating a 60Y F patient
Intubating a 60Y F patient
Signup and view all the flashcards
Minimal occlusion test
Minimal occlusion test
Signup and view all the flashcards
MLT and MOV
MLT and MOV
Signup and view all the flashcards
Optimal cuff pressure?
Optimal cuff pressure?
Signup and view all the flashcards
Adjusted but NOT Main settings of MV
Adjusted but NOT Main settings of MV
Signup and view all the flashcards
I-time Increased & Flow Constant
I-time Increased & Flow Constant
Signup and view all the flashcards
Vent circuit (tube) changes?
Vent circuit (tube) changes?
Signup and view all the flashcards
LMA Size
LMA Size
Signup and view all the flashcards
LMA Cuff Pressure
LMA Cuff Pressure
Signup and view all the flashcards
MV Indication
MV Indication
Signup and view all the flashcards
I:E Ratio
I:E Ratio
Signup and view all the flashcards
Consider I:E ratio
Consider I:E ratio
Signup and view all the flashcards
Divide TCT by # parts
Divide TCT by # parts
Signup and view all the flashcards
Influencing Compliance
Influencing Compliance
Signup and view all the flashcards
Dynamic compliance
Dynamic compliance
Signup and view all the flashcards
Static compliance
Static compliance
Signup and view all the flashcards
Basic Graphics on ventilator
Basic Graphics on ventilator
Signup and view all the flashcards
Increase I-time
Increase I-time
Signup and view all the flashcards
Inverse Ratio.
Inverse Ratio.
Signup and view all the flashcards
Total cycle time?
Total cycle time?
Signup and view all the flashcards
MV can
MV can
Signup and view all the flashcards
Intubation
Intubation
Signup and view all the flashcards
MacIntosh and Miller
MacIntosh and Miller
Signup and view all the flashcards
Type I Respiratory Failure
Type I Respiratory Failure
Signup and view all the flashcards
Type II Respiratory Failure
Type II Respiratory Failure
Signup and view all the flashcards
Pressure Support
Pressure Support
Signup and view all the flashcards
Minute Ventilation: Ve = Vt x f
Minute Ventilation: Ve = Vt x f
Signup and view all the flashcards
Tidal Volume (Vt)
Tidal Volume (Vt)
Signup and view all the flashcards
Heat & Humidification
Heat & Humidification
Signup and view all the flashcards
Trigger
Trigger
Signup and view all the flashcards
Cycle
Cycle
Signup and view all the flashcards
Sensitivity
Sensitivity
Signup and view all the flashcards
Normal value.
Normal value.
Signup and view all the flashcards
Study Notes
OPAs (Oropharyngeal Airways) and NPAs (Nasopharyngeal Airways)
- OPAs and NPAs are used to maintain a patent airway
OPA Indications
- Used to maintain an open airway in unconscious patients
Measuring OPAs
- Measure from the corner of the mouth to the earlobe
OPA Procedures
- Inserted into the mouth to prevent the tongue from obstructing the airway
NPA Indications
- Used when the patient requires frequent suctioning
Measuring NPAs
- Measure from the tip of the nose to the earlobe
NPA Procedures
- Inserted into the nose to prevent the tongue from obstructing the airway
Airway Considerations
- OPAs is contraindicated when a patient has a gag reflex
- NPAs are appropriate for repeated suctioning
- OPA measurement is from the corner of the mouth to the earlobe
- Neither OPAs nor NPAs should be used during bag mask ventilation
LMA (Laryngeal Mask Airway)
- Adult size is usually 4 to 5
- Cuff pressure should be approximately 50 cmH2O
LMA Indications
- Used as an alternative airway device in appropriate clinical scenarios
LMA Insertion
- Inserted into the pharynx to create a seal around the larynx
Indications for MV (Mechanical Ventilation)
- Respiratory failure (pH < 7.25)
- Possibly impending failure may also necessitate MV
- Prophylactic reasons such as post surgery
- Neuro diseases/injuries
- Epiglottitis
- Neuromuscular diseases
- Ventilation failure
- Oxygenation failure
- Respiratory distress
Mechanical Ventilation Indications
- Ventilation management for patients with closed head trauma and increasing ICP
- Epiglottitis in a 4-year-old
- pH of 7.18
- Respiratory distress
ET Tubes (Endotracheal Tubes)
- Crucial to understand characteristics of ET Tubes
Common Adult ET Tube Sizes
- Variable for females compared to males
ET Tube Cuff Pressures
- Need to know Maximum pressures
- MLT (Minimal Leak Technique)
- MOV (Minimal Occlusion Volume)
Intubation
- Essential to understand different blade types
Intubation Blade Types
- MacIntosh
- Miller
Intubation Sizes
- Must know about various sizes of ET Tubes
Intubation Techniques
- Essential for successful airway management
Managing ET Tube Leaks
- For a 35-year-old female on mechanical ventilation with a 6.5 ET tube, first check the cuff pressure and adjust to a maximum of 30 cmH2O if there's a leak around the ET tube
Intubating a Patient
- For a 60-year-old female patient who is 5'8" and 88 kg, use a Mac 3.0 blade and ETT size 7.0, placing the blade in the vallecula
Minimal Leak Test (MLT) and Minimal Occlusion Volume (MOV) Test
- In the MLT, inflate the cuff until a small leak is heard at the end of inspiration
- In the MOV test, inflate until there is no perceptible leak
- These tests are not typically applied to tracheostomy tubes
- The ideal pressure with either test is 20 – 30 cmH2O
Objectives of MV
- Improve ventilation before improving oxygenation, decrease the work of breathing (WOB), improve acid-base imbalances, and assist in improving metabolic issues
- MV primarily compensates and does not improve metabolic issues
Main Settings of MV
- Tidal volume (Vt), respiratory rate (f), FiO2, and PEEP
Additional MV Settings
- PIP, MAP, Ve, triggers & cycles, and alarms are helpful to control but are not "main settings"
Heat and Humidification
- Use HMEs (Heat Moisture Exchangers)
Heated Humidifiers
- Typically set at 37°C for ETT or tracheostomy tubes, but may be set at 34°C for mask ventilation
- Need to know the indications for humidification
Controlling Volume on a Ventilator
- Adjust flow, I-time, or pressure
Volume Increase in PC Mode
- Increase the flow or inspiratory time
Constant Volume Control
- If volume delivered by a vent is to remain constant while flow is increased, the time must decrease
MV Terms
- Need to know Trigger, Cycle, Sensitivity, Compliance, Resistance, Volume, Minute Ventilation, MAP, Pressure, Barotrauma, and Volutrauma
Minute Ventilation Formula
- Ve = Vt x f
Barotrauma
- Excessive pressure & lung injury outside the alveoli
Volutrauma
- Injury to the alveoli
Ventilation Statements
- A trigger starts a breath
- A cycle ends an inspiratory phase
- Minute ventilation can only be adjusted by changing tidal volume
- Sensitivity describes how easy or how difficult it is to initiate a breath
Managing High Vt
- For a high Vt (12ml/kg) prescription, ask the physician to change the order to 10 ml/kg and decrease the rate to prevent barotrauma/volutrauma
Two Categories of MV
- Volume Control
- Pressure Control
PEEP (Positive End-Expiratory Pressure)
- Increases FRC
PEEP Effects
- PEEP will improve a patient’s FRC and improve oxygenation
Volume, Flow, and Time Relationship
- Flow/60 = Vt/I-time
Pressure Limit
- Designed to limit P-peak but does not cycle the breath
Initial Ventilator Settings
- Modes
- Vt
- Rate
- FiO2
- I:E
Initial MV Settings
- To initiate MV on a 6'1" female, 88 kg, at 6 ml/kg who has overdosed, start with CMV, Vt 400, f 20
TCT (Total Cycle Time)
- The time from the start of one breath to the start of the next
TCT Calculation
- 60 / Rate
I:E Ratio
- Ratio of inspiration to expiration
- Normal is 1:3
- For restrictive diseases consider 1:2
- For COPD consider 1:4 to 1:6
Calculating I-time or E-time
- Add the I:E ratio to get the number of parts, then divide TCT by # parts
Quick I:E Ratio calculation
- Simply divide E-time by I-time
Inverse Ratio Indications
- When conventional ventilation strategies are failing
Common I:E Ratios
- 2:1, 3:1
Pressure Support
- Related to spontaneous breaths; supports during inspiration
- May be a stand-alone mode (PSV) or combined with SIMV or CPAP
Pressure Support
- Pressure support may be used for either CPAP or SIMV modes.
- PSV supports spontaneous breaths
Pressure Support Setting
- Setting P/S for spontaneous breaths in A/C is not universally true
Major Modes
- CMV, A/C, IMV, SIMV, PSV, CPAP, BiPAP need to be understood for their characteristics
Compliance
- There are two types Static and Dynamic
Static Compliance
- Cstat = Vt / (Pplat – PEEP)
Dynamic Compliance
- Cdyn = Vt / (PIP – PEEP)
Factors Influencing Compliance
- "Stiffness" of the lungs (e.g., fibrosis)
- Muscular tension
- Secretions & fluid in the lungs
- Alveolar surface tension
P/F Ratio
- The ratio of PaO2 to FiO2 and is computed by PaO2 / FiO2
- < 300 may indicate ALI
- < 200 may indicate ARDS
Dynamic Compliance
- Dynamic compliance considers airway resistance and the elastic properties of the lungs
Static Compliance Measurement
- Static compliance is measured when flow is momentarily stopped
- Norm values: Dynamic - 30 to 40 ml/cmH2O and Static - 40 to 60 ml/cmH2O
- Dynamic compliance would be significantly different in a fibrosis patient compared to a COPD patient
Basic Graphics on Ventilators
Scalars
- Real-time displays of pressure, volume, and flow
Loops
- Graphs of pressure-volume and flow-volume relationships
Air-trapping
- Recognizing signs of air-trapping
Pressure Triggers
- How pressure triggers work
Respiratory Failure
- Includes Type I and Type II
Type I Respiratory Failure
- Decreased O2 (Hypoxemia)
Type II Respiratory Failure
- Decreased O2 and increased CO2 (Hypercapnia)
Indications of Respiratory Failure
- VC < 15 ml/kg
- Vt - < 3 to 5 ml/kg
- RR - > 30 bpm &/or labored or irregular
- Ve - > 10L/min
- MIP (NIP) - < -20 cmH2O
- PaCO2 - > 50 mmHg (unless CO2 retainer)
- pH - < 7.25
WOB/SOA with ABGs
- For a patient with WOB/SOA and ABGs of pH 7.47, PaCO2 32, PaO2 48, HCO3 25 related to fluid overload, treatment should be diuresis
Increased I-time
- If I-time increases and flow remains constant, Vt will increase
Vent Circuit Changes
- Avoid venting unless there is a pin-hole leak
- It is not necessary to change the circuit for secretions that have accumulated in the circuit since they are from the patient.
- The RT may elect to clamp the ETT if a circuit change is necessary
Indicators of Respiratory Failure
- A vital capacity of 6.5 ml/kg
- A respiratory rate of 20
- A minute ventilation of 12 L/min
- A P/F Ratio of 120
- A tidal volume of 4 ml/kg
Prophylactic Intubation
- For a 5'4" 68 kg female patient being prophylactically intubated, consider CMV, Vt 400, f 12, PEEP 5, FiO2 0.60
Post Intubation
- To obtain a compensated pH with a PaCO2 of 40 torr, raise the Vt to 500 and maintain the f at 14
- If you wish to raise the Vt up to 500 with post intubation ABG
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Related Documents
Description
Overview and indications for using Oropharyngeal Airways (OPAs) and Nasopharyngeal Airways (NPAs). Includes measurements, procedures, and airway considerations for effective airway management. Also covers Laryngeal Mask Airway (LMA) adult sizes and cuff pressure.