Podcast Beta
Questions and Answers
What is the primary healing time for superficial corneal abrasions?
Which of the following is NOT a common cause of superficial corneal abrasions?
What is a likely symptom of a corneal abrasion?
What is the recommended first-line antibiotic for treating corneal abrasions?
Signup and view all the answers
What type of staining is expected in a superficial corneal abrasion?
Signup and view all the answers
If a patient experiences a mild anterior chamber reaction, what is the recommended treatment?
Signup and view all the answers
What should be done if the corneal abrasion is related to contact lens wear?
Signup and view all the answers
Which of the following signs indicates a superficial corneal abrasion?
Signup and view all the answers
What is the potential duration for healing of Basal layer damage from a corneal abrasion?
Signup and view all the answers
Which treatment option is not recommended for pain management in corneal abrasions?
Signup and view all the answers
What is a potential cause of deep abrasions?
Signup and view all the answers
Which symptom is NOT associated with deep abrasions?
Signup and view all the answers
What does a positive NaFL indicate in cases of deep abrasions?
Signup and view all the answers
Which treatment should be avoided for deep abrasions?
Signup and view all the answers
In assessing deep abrasions, what does an irregular, 'grainy' NaFL pattern indicate?
Signup and view all the answers
What is the recommended management for a deep abrasion when anterior chamber reactions are moderate to severe?
Signup and view all the answers
What should be done if there is a concern for penetration or perforation of the cornea?
Signup and view all the answers
How often should 5% NaCl be administered if significant edema is present following a deep abrasion?
Signup and view all the answers
Which of the following indicates corneal edema in the context of deep abrasions?
Signup and view all the answers
What is the defining characteristic of a stromal channel in cases of corneal injury?
Signup and view all the answers
What is the primary management strategy for a corneal condition related to contact lens wear?
Signup and view all the answers
Which of the following statements is TRUE regarding corneal degenerations?
Signup and view all the answers
Arcus senilis is characterized by which feature?
Signup and view all the answers
In corneal degenerations, which group of patients is most likely to experience arcus senilis?
Signup and view all the answers
Which treatment option is suggested for managing pain related to corneal issues?
Signup and view all the answers
What can result from corneal degenerations, particularly in older patients?
Signup and view all the answers
Which intervention may be added for edema in corneal issues?
Signup and view all the answers
What is true about the genetic factors in most corneal degenerations?
Signup and view all the answers
If a deep abrasion does not heal within a week, which factor should be considered as a possible influence?
Signup and view all the answers
What is a common characteristic of corneal degenerations?
Signup and view all the answers
Study Notes
Keratitis by Injury
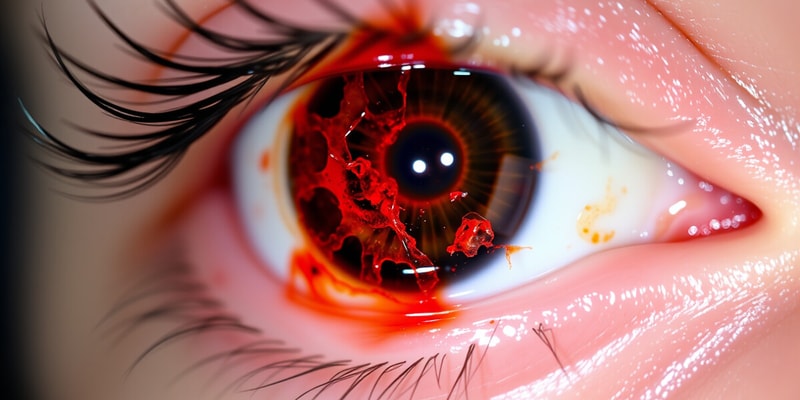
Corneal Abrasions
- Loss of epithelial cells due to injury, classified as superficial or deep.
-
Superficial Abrasion:
- Involves loss of superficial/squamous cells.
- Healing time: hours to 1 day.
-
Deep Abrasion:
- Loss extends to basal cell layer or basement membrane (BM).
- Healing time: 3-4 days to a week; BM damage can take 8-12 weeks.
Superficial Abrasion Causes and Symptoms
- Common causes:
- Transient foreign bodies (FB), mascara, blunt trauma, contact lens overuse, nails, plants, EBMD, corneal dystrophies.
- Symptoms include:
- Pain, photophobia, foreign body sensation (FBS), tearing, scratch history.
Superficial Abrasion Signs and Work-up
- Signs include:
- Positive NaFL stain with diffuse light; no pooling or deep staining (BM).
- Conjunctival injection, mild eyelid and corneal edema, mild anterior chamber reaction.
- Work-up involves:
- Detailed patient history, lid eversion for FB, irrigation with saline, rule out traumatic uveitis.
Superficial Abrasion Treatment
- Always irrigate in-office with sterile saline.
- Antibiotics:
- First-line: Polytrim; if lens wear leads to abrasion, switch to fluoroquinolone.
- Other options: aminoglycoside.
- Pain management:
- Mild A/C reaction: Cyclopentolate 1% BID; topical NSAIDs (oral alternatives if follow-up is imminent).
- Schedule follow-up every 2-3 days.
- Do not patch an abrasion.
Deep Abrasions
- Detailed injury causes include fingernails, paper cuts, flying materials, tree branches, mascara brushes.
- Symptoms: pain, photophobia, blepharospasm, tearing.
- Signs:
- Lid edema, positive NaFL pooling or deep staining, corneal edema, epithelial tags.
Deep Abrasion Work-up and R/O
- Assess severity by measuring and determining cell layers involved.
- Identify epithelial tags and irregular NaFL patterns.
- Rule out perforation, endothelial disruption, and foreign materials.
- Refer to a corneal specialist if perforation is suspected.
Deep Abrasion Treatment
- Antibiotics: Polytrim, fluoroquinolone; avoid aminoglycoside due to corneal toxicity.
- Moderate to severe A/C reactions: Homatropine 5% TID for cycloplegia.
- Pain management with topical NSAIDs; may consider 5% NaCl for significant edema.
- Bandage contact lenses may be used for abrasions >10 mm (if no vegetative material).
- Daily follow-up is necessary for lens-related abrasions.
Corneal Degenerations/Dystrophies
- Changes in corneal tissue leading to deterioration can impair visual function and clarity.
Corneal Degenerations
- Commonly unilateral, can be asymmetric if bilateral.
- Result from involutional (age-related) changes or systemic diseases without hereditary factors.
- Most often found in the periphery of the cornea; may lead to thinning, vascularization, or material deposition.
- Late-onset changes.
Arcus Senilis
- Involutional condition characterized by a white ring in the peripheral cornea.
- Originates inferiorly, extends superiorly to create a complete ring.
- Clear interval between limbus and arcus; involves Bowman’s layer.
- Consists of accumulated cholesterol, triglycerides, and phospholipids.
- Found in 60% of individuals aged 40-60, and 100% in those over 80; typically not related to hyperlipidemia past age 40.
- No management is needed for individuals older than 40 unless symptomatic.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Related Documents
Description
This quiz covers the causes, symptoms, and signs related to corneal abrasions resulting from injury. It differentiates between superficial and deep abrasions, detailing their healing times and associated symptoms. Test your knowledge on the diagnosis and management of keratitis due to injury.