Podcast
Questions and Answers
Which of the following correctly describes the passive nature of glomerular filtration?
Which of the following correctly describes the passive nature of glomerular filtration?
What is the primary function of tubular reabsorption in the nephron?
What is the primary function of tubular reabsorption in the nephron?
How is the Glomerular Filtration Rate (GFR) primarily regulated?
How is the Glomerular Filtration Rate (GFR) primarily regulated?
What is the net filtration pressure (NFP) typically in the glomerulus?
What is the net filtration pressure (NFP) typically in the glomerulus?
Signup and view all the answers
In terms of hormonal regulation, what does a decrease in renal blood pressure trigger?
In terms of hormonal regulation, what does a decrease in renal blood pressure trigger?
Signup and view all the answers
Why are the afferent arterioles significant in maintaining glomerular blood pressure?
Why are the afferent arterioles significant in maintaining glomerular blood pressure?
Signup and view all the answers
What is the role of tubular secretion in the renal system?
What is the role of tubular secretion in the renal system?
Signup and view all the answers
What is one consequence of sympathetic activity on GFR?
What is one consequence of sympathetic activity on GFR?
Signup and view all the answers
Which statement regarding the characteristics of glomerular filtration is incorrect?
Which statement regarding the characteristics of glomerular filtration is incorrect?
Signup and view all the answers
What is the primary role of the tubule in tubular secretion?
What is the primary role of the tubule in tubular secretion?
Signup and view all the answers
Which of the following is NOT a function of tubular secretion?
Which of the following is NOT a function of tubular secretion?
Signup and view all the answers
What is the main site for the secretion of substances in the kidney?
What is the main site for the secretion of substances in the kidney?
Signup and view all the answers
Which physiological process is associated with the relaxation of detrusor muscle?
Which physiological process is associated with the relaxation of detrusor muscle?
Signup and view all the answers
Which neurotransmitter is primarily involved in parasympathetic stimulation of detrusor contraction?
Which neurotransmitter is primarily involved in parasympathetic stimulation of detrusor contraction?
Signup and view all the answers
What role does ATP play in the urothelium?
What role does ATP play in the urothelium?
Signup and view all the answers
Which structure is involved in voluntary control of micturition?
Which structure is involved in voluntary control of micturition?
Signup and view all the answers
What occurs to the bladder during the storage phase of urine?
What occurs to the bladder during the storage phase of urine?
Signup and view all the answers
Which of the following is a consequence of sympathetic stimulation in the bladder?
Which of the following is a consequence of sympathetic stimulation in the bladder?
Signup and view all the answers
Which component of the bladder is directly responsible for expelling urine?
Which component of the bladder is directly responsible for expelling urine?
Signup and view all the answers
What is the primary function of the glomerulus in the nephron?
What is the primary function of the glomerulus in the nephron?
Signup and view all the answers
Which statement best describes the role of the juxtaglomerular apparatus?
Which statement best describes the role of the juxtaglomerular apparatus?
Signup and view all the answers
What is meant by the transport maximum in renal physiology?
What is meant by the transport maximum in renal physiology?
Signup and view all the answers
Which hormones are primarily involved in the regulation of kidney functions?
Which hormones are primarily involved in the regulation of kidney functions?
Signup and view all the answers
How is tubular reabsorption different from glomerular filtration?
How is tubular reabsorption different from glomerular filtration?
Signup and view all the answers
What triggers the release of renin from the juxtaglomerular cells?
What triggers the release of renin from the juxtaglomerular cells?
Signup and view all the answers
What is the consequence of renal autoregulation?
What is the consequence of renal autoregulation?
Signup and view all the answers
What substances are primarily lost during the urine formation process in the collecting ducts?
What substances are primarily lost during the urine formation process in the collecting ducts?
Signup and view all the answers
In which part of the nephron does the majority of tubular reabsorption occur?
In which part of the nephron does the majority of tubular reabsorption occur?
Signup and view all the answers
What role does the peritubular capillary network serve in kidney function?
What role does the peritubular capillary network serve in kidney function?
Signup and view all the answers
What effect does hyperglycemia have on transport maximum (TM) in uncontrolled diabetes mellitus?
What effect does hyperglycemia have on transport maximum (TM) in uncontrolled diabetes mellitus?
Signup and view all the answers
Which hormone primarily regulates sodium reabsorption in the distal convoluted tubule?
Which hormone primarily regulates sodium reabsorption in the distal convoluted tubule?
Signup and view all the answers
What is the primary mechanism by which Na+ is reabsorbed in the proximal convoluted tubule?
What is the primary mechanism by which Na+ is reabsorbed in the proximal convoluted tubule?
Signup and view all the answers
What role do aquaporins play during the reabsorption process in the Loop of Henle?
What role do aquaporins play during the reabsorption process in the Loop of Henle?
Signup and view all the answers
How does anti-diuretic hormone (ADH) function in the regulation of water reabsorption?
How does anti-diuretic hormone (ADH) function in the regulation of water reabsorption?
Signup and view all the answers
What happens to tubular reabsorption when atrial natriuretic peptide (ANP) is released?
What happens to tubular reabsorption when atrial natriuretic peptide (ANP) is released?
Signup and view all the answers
Which of the following accurately describes the role of renal autoregulation?
Which of the following accurately describes the role of renal autoregulation?
Signup and view all the answers
What mechanism is primarily responsible for the reabsorption of organic nutrients in the renal system?
What mechanism is primarily responsible for the reabsorption of organic nutrients in the renal system?
Signup and view all the answers
Which ion's reabsorption is coupled with the reabsorption of water through osmosis?
Which ion's reabsorption is coupled with the reabsorption of water through osmosis?
Signup and view all the answers
What triggers the release of aldosterone from the adrenal cortex?
What triggers the release of aldosterone from the adrenal cortex?
Signup and view all the answers
Which substance is primarily removed from the body through tubular secretion?
Which substance is primarily removed from the body through tubular secretion?
Signup and view all the answers
What physiological change occurs in the detrusor muscle during bladder filling?
What physiological change occurs in the detrusor muscle during bladder filling?
Signup and view all the answers
What is the main physiological role of urothelial signaling mediators?
What is the main physiological role of urothelial signaling mediators?
Signup and view all the answers
How does sympathetic stimulation affect the bladder during urine storage?
How does sympathetic stimulation affect the bladder during urine storage?
Signup and view all the answers
Which structure is primarily involved in the coordination of bladder functions?
Which structure is primarily involved in the coordination of bladder functions?
Signup and view all the answers
What is the function of the micturition reflex?
What is the function of the micturition reflex?
Signup and view all the answers
What role do ion channels play in the urothelium?
What role do ion channels play in the urothelium?
Signup and view all the answers
Which type of nerve stimulation primarily causes detrusor contraction during urination?
Which type of nerve stimulation primarily causes detrusor contraction during urination?
Signup and view all the answers
What is the primary effect of the detrusor muscle during bladder micturition?
What is the primary effect of the detrusor muscle during bladder micturition?
Signup and view all the answers
What is the role of mediators like nitric oxide in the bladder?
What is the role of mediators like nitric oxide in the bladder?
Signup and view all the answers
What is a primary function of the urinary system related to blood composition?
What is a primary function of the urinary system related to blood composition?
Signup and view all the answers
Which part of a nephron is responsible for the filtration of blood?
Which part of a nephron is responsible for the filtration of blood?
Signup and view all the answers
In which segment of a nephron does the majority of solute reabsorption occur?
In which segment of a nephron does the majority of solute reabsorption occur?
Signup and view all the answers
What occurs during tubular secretion in the nephron?
What occurs during tubular secretion in the nephron?
Signup and view all the answers
What role do sympathetic nerves primarily play in micturition?
What role do sympathetic nerves primarily play in micturition?
Signup and view all the answers
Which hormone is involved in the management of blood pressure by the kidneys?
Which hormone is involved in the management of blood pressure by the kidneys?
Signup and view all the answers
What distinct characteristic does the juxtamedullary nephron have?
What distinct characteristic does the juxtamedullary nephron have?
Signup and view all the answers
How does the macula densa contribute to kidney function?
How does the macula densa contribute to kidney function?
Signup and view all the answers
Which statement best describes urine composition after it is formed in the collecting ducts?
Which statement best describes urine composition after it is formed in the collecting ducts?
Signup and view all the answers
What effect does parasympathetic stimulation have on the detrusor muscle of the bladder?
What effect does parasympathetic stimulation have on the detrusor muscle of the bladder?
Signup and view all the answers
What primarily drives the process of glomerular filtration?
What primarily drives the process of glomerular filtration?
Signup and view all the answers
Which substance is least likely to be found in the glomerular filtrate due to its size?
Which substance is least likely to be found in the glomerular filtrate due to its size?
Signup and view all the answers
During tubular reabsorption, which of the following processes occurs?
During tubular reabsorption, which of the following processes occurs?
Signup and view all the answers
Which of the following best defines tubular secretion?
Which of the following best defines tubular secretion?
Signup and view all the answers
What is the primary function of the efferent arterioles in the glomerulus?
What is the primary function of the efferent arterioles in the glomerulus?
Signup and view all the answers
The Glomerular Filtration Rate (GFR) can be affected by which of the following factors?
The Glomerular Filtration Rate (GFR) can be affected by which of the following factors?
Signup and view all the answers
What is the typical range for Glomerular Filtration Rate (GFR) in adults?
What is the typical range for Glomerular Filtration Rate (GFR) in adults?
Signup and view all the answers
Which mechanism does sympathetic activity primarily use to influence GFR?
Which mechanism does sympathetic activity primarily use to influence GFR?
Signup and view all the answers
The term Net Filtration Pressure (NFP) takes into account which of the following pressures?
The term Net Filtration Pressure (NFP) takes into account which of the following pressures?
Signup and view all the answers
In renal physiology, what is the significance of the renin-angiotensin mechanism?
In renal physiology, what is the significance of the renin-angiotensin mechanism?
Signup and view all the answers
What is the primary mechanism of sodium reabsorption in the proximal convoluted tubule?
What is the primary mechanism of sodium reabsorption in the proximal convoluted tubule?
Signup and view all the answers
How does aldosterone primarily affect sodium reabsorption in the kidneys?
How does aldosterone primarily affect sodium reabsorption in the kidneys?
Signup and view all the answers
What is the consequence of excess glucose exceeding the transport maximum (TM) in the renal tubules?
What is the consequence of excess glucose exceeding the transport maximum (TM) in the renal tubules?
Signup and view all the answers
Which hormone inhibits both sodium and water reabsorption in the kidneys?
Which hormone inhibits both sodium and water reabsorption in the kidneys?
Signup and view all the answers
What is the role of osmoreceptors in the regulation of anti-diuretic hormone (ADH)?
What is the role of osmoreceptors in the regulation of anti-diuretic hormone (ADH)?
Signup and view all the answers
During which part of tubular reabsorption does water not follow solutes such as sodium?
During which part of tubular reabsorption does water not follow solutes such as sodium?
Signup and view all the answers
What triggers the release of anti-diuretic hormone (ADH) from the posterior pituitary?
What triggers the release of anti-diuretic hormone (ADH) from the posterior pituitary?
Signup and view all the answers
Which of the following substances reabsorption is NOT closely regulated by hormones?
Which of the following substances reabsorption is NOT closely regulated by hormones?
Signup and view all the answers
In what way do peritubular capillaries assist tubular reabsorption?
In what way do peritubular capillaries assist tubular reabsorption?
Signup and view all the answers
Which mechanism describes how cations and organic nutrients are reabsorbed along with sodium?
Which mechanism describes how cations and organic nutrients are reabsorbed along with sodium?
Signup and view all the answers
Study Notes
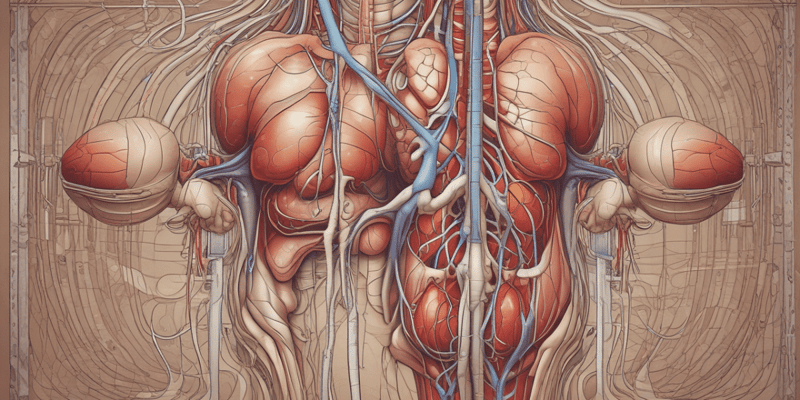
Introduction to the Urinary System
- The urinary system is responsible for removing waste products from the body.
- It regulates blood volume and chemical composition, including water, salts, acids, and bases.
- It produces hormones like renin and erythropoietin.
- It metabolizes vitamin D to its active form.
- It performs gluconeogenesis.
Learning Objectives
- Renal Physiology
- Glomerular filtration
- Tubular reabsorption and secretion
- Urine formation
- Control of bladder filling and micturition
Lecture Learning Outcomes
- Describe the functions of the urinary system
- Describe the structure of kidneys
- Explain the process of glomerular filtration
- Explain the process of tubular reabsorption and tubular secretion
- Explain the role of sympathetic, parasympathetic, and somatic nerves in controlling micturition
Urinary System Functions
- Excretion: Removal of waste products from the body
-
Regulation:
- Blood volume and chemical composition (water, salts, acids, and bases)
- Blood pressure
- Production of hormones: Renin, erythropoietin
- Metabolism: Vitamin D to active form, gluconeogenesis
The Nephron
- Structural and functional units of the kidney
- Over 1 million per kidney
- Glomerular/Bowman's capsule: Surrounds the glomerulus
-
Renal tubule:
- Proximal convoluted tubule (PCT)
- Loop of Henle (descending and ascending limbs)
- Distal convoluted tubule (DCT)
- Collecting duct
The Nephron (detailed)
- Proximal convoluted tubule: Reabsorption of water, ions, organic nutrients
- Glomerulus: Site of filtration
- Efferent arteriole: Smaller diameter, maintains glomerular blood pressure
- Bowman's capsule: Site of filtration
- Capsular space: Fluid enters this space from the glomerulus
- Renal corpuscle: Glomerulus and the Bowman's capsule together
- Loop of Henle: Further reabsorption of water (descending limb), and sodium & chloride (ascending limb)
- Distal convoluted tubule: Variable reabsorption of water, sodium ions and calcium ions
- Collecting ducts: Variable reabsorption of water and the secretion of ions (Na+, K+, H+, HCO3)
- Cortical nephrons: 85% of nephrons, small portion of Loop of Henle projects into outer medulla
- Juxtamedullary nephrons: 15% of nephrons; arise near cortex-medullary junction, important in producing concentrated urine; loops of Henle deeply invade medulla; important in concentrating urine
Nephron Capillary Beds
- Glomerulus: High pressure capillaries, site of filtration, fed and drained by arterioles (afferent and efferent)
- Peritubular capillaries: Low pressure porous capillaries; arise from efferent arteriole, readily reabsorb water and solutes from filtrate into blood
- Vasa recta: Long straight vessels serving juxtamedullary nephrons
Juxtaglomerular Apparatus
- Region where the distal portion of the ascending limb lies against the afferent arteriole;
- Juxtaglomerular/granular cells: Enlarged smooth muscle cells, secretory granules containing renin, mechanoreceptors sensing BP in afferent arteriole
- Macula densa: Closely packed cells of the ascending limb, chemoreceptors, monitor NaCl changes in the filtrate; vasoconstriction
Kidney Physiology: Urine Formation
- 1200 ml blood flows through glomeruli each minute
- 120-125 ml filtrate is forced into renal tubules
- Filtrate contains valuable materials which get reabsorbed
- What remains is urine (mostly metabolic wastes)
Urine Formation – 3 Processes
- Glomerular Filtration: Blood pressure forces fluids and solutes across glomerular capillaries into the glomerular capsule
- Tubular Reabsorption: Removal of water and useful substances from filtrate into the peritubular capillaries
- Tubular Secretion: Movement of substances from peritubular capillaries into the tubular fluid
Glomerular Filtration (Detailed)
- Passive filtration process
- Small molecules (water, ions, small organic molecules e.g. glucose, amino acids, nitrogenous wastes) move across the filtration membrane from high to low pressure
- Proteins and blood cells remain in the blood
- High pressure, large surface area
Glomerular Filtration Rate (GFR)
- Volume of filtrate formed each minute
- Directly proportional to net filtration pressure (NFP)
- Adults: 120-125 ml/min
-
Regulation of GFR:
- Renal autoregulation: Maintain blood pressure within the kidney.
- Neural control: Sympathetic activity lowers GFR by constricting renal arterioles. Stress/emergency
- Hormonal control: Renin-angiotensin mechanism; ↓ blood pressure leads to the production of angiotensin II, which constricts arterioles
Tubular Reabsorption
- Useful tubule contents are returned to the blood
- Begins in the proximal convoluted tubule (PCT)
- Selective trans-epithelial process
- Healthy human kidney: All glucose & amino acids are reabsorbed
- Water and ion reabsorption is regulated (hormonal control)
- Transport types: Passive diffusion, facilitated diffusion, active transport
Sodium Reabsorption
- Na+ ions are most abundant; almost always by active transport
- Na+ enters tubule cells; then actively transported across basolateral membrane via Na+/K+-ATPase pumps
- Na+ and water are rapidly taken up by adjacent peritubular capillaries.
- Active pumping of Na+ drives reabsorption:
- Water (osmosis)
- Cations, fat-soluble substances
- Organic nutrients, cations via secondary active transport (symport or antiport)
Transport Maximum (Tm)
- Reflects the number of transport proteins in the renal tubule and is the limit to how fast reabsorption can happen.
- Substances that are reabsorbed using transport proteins have a maximum value (Tm).
- High Tm value means plenty of carriers. Ex. glucose, amino acids). If exceeded, substances are excreted in urine
- e.g. Hyperglycemia with uncontrolled diabetes mellitus.
Reabsorption in PCT
- Reabsorbs nutrients, ions, water, urea, small proteins
Reabsorption in Loop of Henle
- Tubule permeability changes
- Water reabsorption in the descending limb.
- Different parts of the loop of Henle reabsorb different substances.
- Opposite is true for ascending limb.
Reabsorption in DCT and Collecting Duct
- Reabsorption is dependent on body's specific needs
- Regulated by hormones (aldosterone, ADH, ANP, and parathyroid hormone (PTH)).
Reabsorption: Hormonal Regulators
- Anti-diuretic hormone (ADH): Hypothalamic neurons and osmoreceptors monitor solute concentrations; targets collecting ducts via cAMP system. Water is reabsorbed
- Other stimuli include: pain, low blood pressure, drugs (nicotine, barbiturates, morphine)
- Alcohol inhibits ADH release
- Aldosterone: Adrenal cortex releases aldosterone in response to ↓ blood volume or BP, or low extracellular Na+, or high extracellular K+; regulates fine-tuning reabsorption of Na+.
- Atrial natriuretic peptide (ANP): Specialized cardiac muscle cells in the atria release ANP. Increased blood pressure inhibits the renin-angiotensin system and release of aldosterone. Inhibits Na+ and water reabsorption. ↓ blood volume and BP.
Tubular Secretion
- Substances move from capillaries to renal tubule. Substances not already filtered, or wastes, are secreted
- Essential for:
- Removing substances not already filtered (Drugs, metabolic wastes, drugs)
- Eliminating waste products (urea, uric acid)
- Controlling blood pH (e.g. H+ and HCO3)
- PCT is the main site for secretion (except for K+)
Function & Regulation of the Urinary Bladder
- Hollow, distensible muscular organ that acts as a temporary reservoir for urine.
Bladder
- Hollow, distensible muscular organ.
- Ureteral openings
- Trigone
- Neck of urinary bladder
- Internal urethral sphincter
- External urethral sphincter
The Urothelium
- Inner epithelial layer
- Continuous with the ureters and urethra
- Originally thought to only act as a barrier to water and solutes
- Now known to play an active role in detecting chemical and mechanical stimuli. It has receptors similar to those of afferent nerves.
- Releases mediators stimulating tissue response.
Urothelial Signalling Mediators
- ATP
- Acetylcholine
- PGE2
- Nitric oxide
- Urothelial derived inhibitory factor (UDIF)
Detrusor Muscle
- Contraction of bladder muscle responsible for expulsion of urine.
- During filling, detrusor cells relax and elongate.
Innervation of the Bladder
- Efferent nerves: Sympathetic (relaxation, contraction of bladder neck/internal urethral sphincter), parasympathetic (contraction of detrusor).
- Hypogastric nerve
- Pelvic nerve (parasympathetic)
- Pudendal nerve (somatic innervation, voluntary control)
The Physiology of Storage and Micturition
- Phases of bladder storage and micturition, coordinated by afferent and efferent nerves.
- Storage: Urine accumulates; bladder expands; stretches thin walls; rugae disappear; detrusor muscle relaxes; internal and external urethral sphincters are closed
- Micturition: Normal volume: 400-500 ml
Neural Control: Storage
- Noradrenaline causes bladder relaxation
- Noradrenaline causes internal sphincter contraction
Micturition/Urination
- The act of emptying the bladder.
- Requires detrusor muscle contraction, relaxation of internal and external urethral sphincters;
- Afferent stretch receptors relay bladder fullness to the pons
- Pontine micturition center ↑ parasympathetic and ↓ sympathetic lower urinary tract
Neural Control: Voiding
- Acetylcholine causes bladder contractions; ATP co-released
- Nitric oxide relaxes the urethra
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Related Documents
Description
This quiz covers essential aspects of the urinary system, including its functions such as waste removal and regulation of blood volume. It also explores renal physiology concepts like glomerular filtration and bladder control mechanisms. Test your understanding of the urinary system's role in hormone production and metabolism.